
Long NHS waiting lists are the most common reason for people opting for independent healthcare or considering using the private sector, a poll suggests.
The survey by Ipsos found that while just over six-in-10 people were neither using or planning to use private health services, about a third were either using private care or considering it within the next six months.
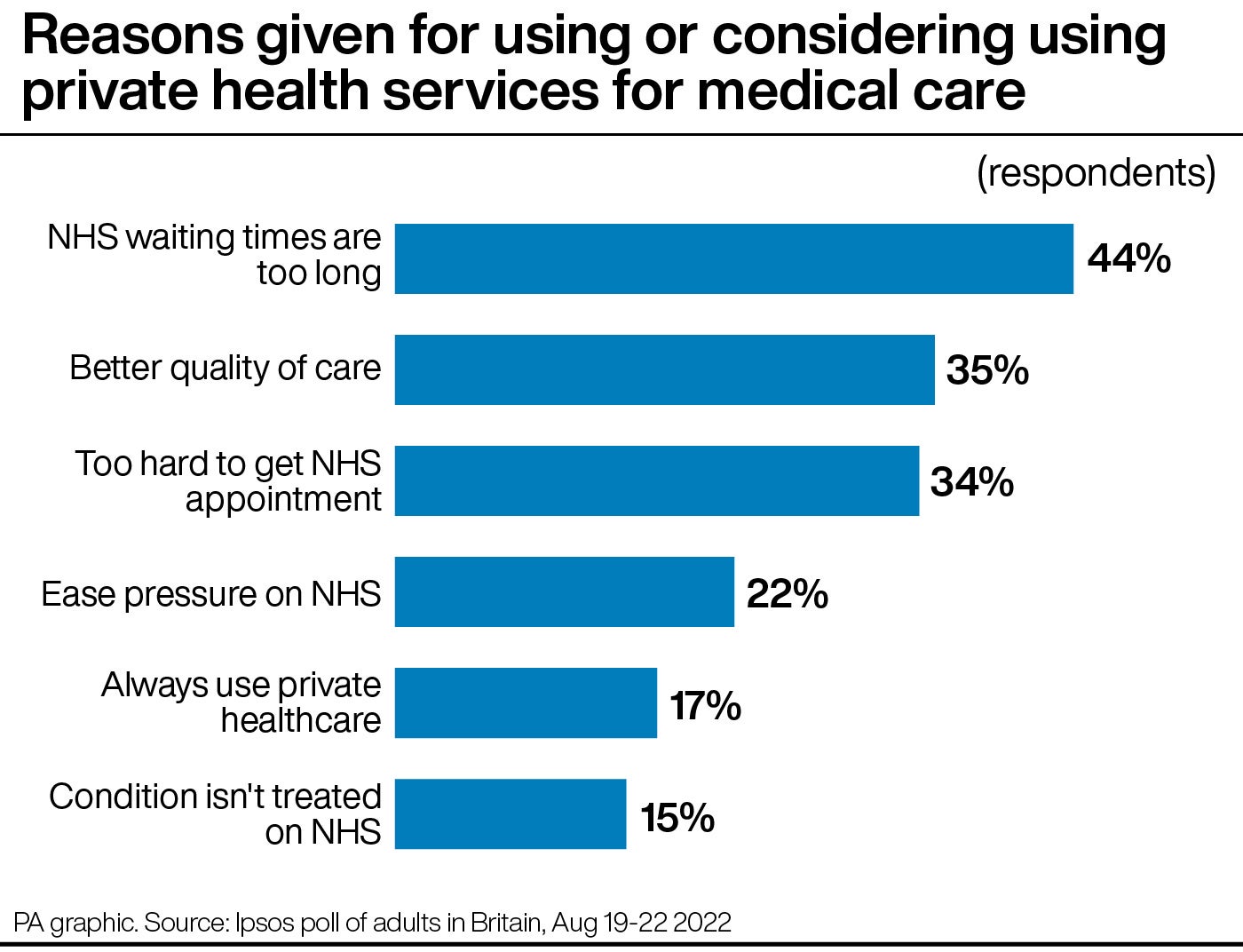
Of those, 44% said the main reason for this was NHS waiting times were too long, followed by about a third (35%) who said the quality of care will be, or is, better.
Some 43% said they found it too hard to get an NHS appointment, while a fifth (22%) said it was to ease the pressure on the NHS.
The latest NHS England figures show that the number of people in England waiting for routine hospital treatments stood at a record 6.7 million at the end of June.
Health experts have said the record NHS backlog could be fuelling growing demand for private care, with data showing a 29% rise in people paying for healthcare out of their own pockets in 2021 compared to before the pandemic in 2019.
David Hare, chief executive of the Independent Healthcare Providers Network (IHPN), said that with waiting lists expected to grow, it was not surprising more people were considering paying for private treatment.
Jonathon Holmes, policy adviser at the King’s Fund, said it was “concerning” to see so many people considering using private treatments.
He added: “It suggests the performance data we are seeing and the almost systemic performance challenges across the NHS are clearly having a very tangible impact on people’s experience of care and are seeing the principle of NHS universality – free at the point of use – is not happening.”
Health leaders have warned that the Government cannot allow the creation of a two-tier health system with those who can afford it going private while others are forced to wait for NHS care.
Matthew Taylor, chief executive of the NHS Confederation, said that whoever becomes Prime Minister next week must be ready to give the NHS the support it needs.
He added: “The NHS is in this dire situation because it is still reeling from a decade of austerity, continued underinvestment and understaffing, and the devastating consequences of the pandemic.
“The NHS is there for everyone and leaders can see plainly how the last two years have exacerbated health disparities across the country.
“Future Government policy must bear this in mind and not instil a two-tier system in the NHS based on affordability that could put people off from seeking the help they need when they need it.”
The Ipsos poll of 2,104 British adults also found that 45% of people would be less likely to seek routine medical care if there was a £8 charge for an overnight stay in hospital.
This was a suggestion made by former hospital boss Professor Stephen Smith, who said patients could be charged £4 to £8 to help cover the costs of medical equipment such as hearing aids and walking devices.
He also suggested people over 60 should start paying for their prescriptions to help raise more revenue.
But the Ipsos poll found that 31% of people said charges for medical devices would put them off, while 47% of people aged 60 and over said prescription charges would make them less likely to seek routine care.
Mr Holmes said that the figures were less of a reflection of whether people would or would not seek care based on charges, but of how important people believe an NHS free at the point of delivery is.
He told the PA news agency: “There will be a very small proportion of the country for whom an £8 charge is prohibitively expensive but for the vast majority of the country I would imagine it would be a cost they would be able to meet.
“But we are seeing a reaction against the idea of charging.
“This is about support for the basic model of the NHS but expressed differently because of the economic and financial context that we find ourselves in.
“The charge may appear nominal but there may be some that are disincentivised from seeking healthcare, particularly with people’s acute needs.”
It is vital that people do not put off seeking care when they need it.— NHS spokeswoman
But Mr Holmes did say that charging for an overnight stay in hospital could put people off seeking urgent or emergency care.
He added: “I would be concerned that for some people it would act as a disincentive to seek treatment that they need at the earliest possible stage. You might see people unnecessarily choosing to defer seeking medical help which will have a damaging effect on their health in the longer term.”
Louise Ansari, national director at Healthwatch England, said for two-thirds of people choosing to go private was not an option and the rising cost of living could widen inequalities.
She added: “Our evidence also shows that people on the lowest incomes are the most likely to wait the longest for NHS treatment and will have a more negative experience of waiting.
“In turn, this leads to a worse impact on their physical health, mental health and their ability to work and care for loved ones.
“Tackling the NHS backlog is a huge challenge but decision makers must find a way to do so without exacerbating health inequalities, the extent of which has been laid bare by the pandemic.”
An NHS spokeswoman said: “Record numbers of people are being treated by the NHS with waits of more than two years virtually eliminated and those waiting more than 18 months already down by over 20,000 since January – at the same time the NHS is carrying out more cancer checks than ever before, delivering millions more GP appointments compared to before the pandemic and dealing with the highest number of the most serious ambulance call outs in July.
“The message, however, to patients is clear and has not changed – it is vital that people do not put off seeking care when they need it.”
A Department of Health and Social Care spokesman said: “Last week we announced the opening of a further 50 surgical hubs, on top of the 91 that are already open, which will ensure millions of people get the surgery they need.
“This is in addition to the 92 community diagnostic centres which have already delivered almost 1.7 million extra checks, scans and tests.
“The NHS has set out further measures to rapidly boost capacity and resilience ahead of this winter, including boosting NHS 111 and 999 support, tackling delayed hospital discharge and creating the equivalent of at least 7,000 more beds, including through innovative virtual wards.”







