With the first reading of a new bill in parliament today, Aotearoa New Zealand’s plan to be smokefree by 2025 takes another tangible step forward.
The Smokefree Environments and Regulated Products (Smoked Tobacco) Amendment Bill will now go to the Health Select Committee for submissions and review, and (presumably) return to the House in late 2022 to be passed into law.
Assuming the final legislation looks similar to what is being proposed, it will mean Aotearoa New Zealand leapfrogs all other countries to be at the vanguard of tobacco control, with policy settings aimed at getting smoking prevalence beneath 5% of the adult population within years (not decades).
The bill provides for three key strategies:
drastically reducing nicotine content in tobacco so it is no longer addictive (known as “denicotinisation” or “very low nicotine cigarettes” (VLNC))
a 90% to 95% reduction in the number of shops that can sell tobacco
making it illegal to sell tobacco to people born in 2009 or later (thus creating a “smokefree generation”).
If implemented effectively this is anticipated to have a profound impact on smoking.
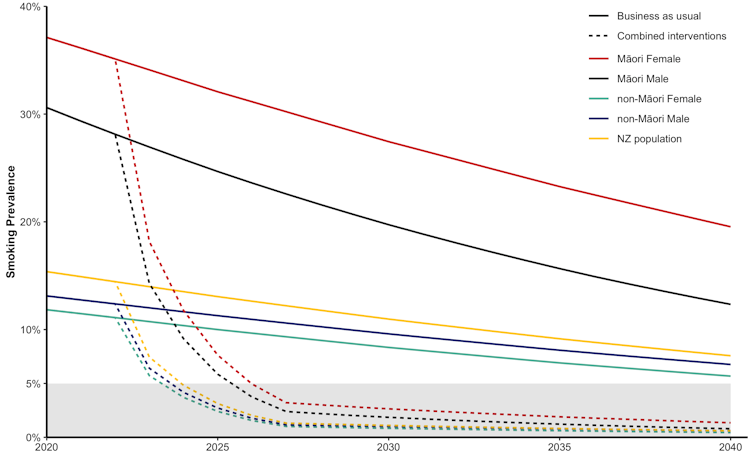
Projected declines in smoking
Reducing Māori health inequity
If successful, this would be a monumental achievement for generations of tobacco-control advocates and researchers. The concept of a “tobacco endgame” will move beyond aspiration and into reality.
We’ve got to this point after decades of Māori leadership, research and advocacy, with the proposed legislation having its roots in the aim of reducing health inequities between Māori and non-Māori. This kaupapa (principle or policy) has driven the process and is supported by Māori communities.
Much more will be written in coming months about this groundbreaking legislation. Here we focus on the modelling we were commissioned to provide by the New Zealand government in 2021-2022 on the potential health and cost impacts of the Smokefree Aotearoa 2025 Action Plan.
Our findings underpinned the regulatory impact statement that set out the options to regulate tobacco products as part of the action plan, which Cabinet considered in early 2022.
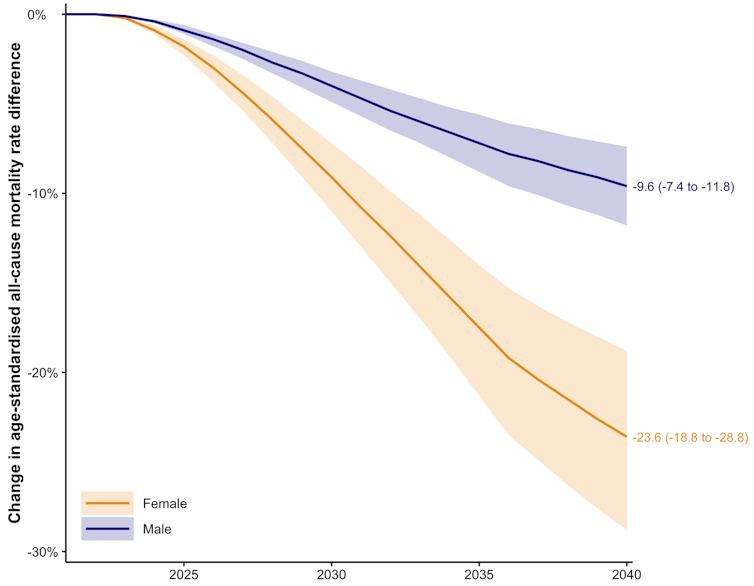
Large reductions in mortality rates
In our work at Otago University’s BODE3 program and the University of Melbourne’s Scalable Health Intervention Evaluation (SHINE) we model many potential public health interventions, from dietary counselling and reducing salt in bread to the evaluation of screening programmes and drug treatments.
We tally the likely health gains from these interventions, and how much they might reduce inequities in health. When we do this for the government’s tobacco endgame strategy, the forecasts are breathtaking.
Consider reductions in health inequities between Māori and non-Māori. First, we forecasted what Māori and non-Māori mortality rates will be in 2040 (and beyond) given trends we have seen in recent decades (business as usual in the graph above).
Second, we estimated how much smoking (and vaping) rates would change into the future for the combined endgame policy (denicotinisation, retail reduction, smokefree generation regulations, augmented by some media promotion of the policy).
Third, allowing for time lags, we modelled future disease rates (for example, lung and heart disease) and then the overall impact on mortality rates.
We then compared the gap between Māori and non-Māori mortality or death rates in 2040 if there were no major policy changes, and under the combined tobacco endgame strategy. For those aged 45 and over, the gap was reduced by a staggering 22.9% for Māori females compared to non-Māori females, and a still very large 9.6% for males.
Projected decline in gap between Māori and non-Māori mortality rates
Longer, healthier lives
In all our previous research, we have never seen a single health intervention with the potential to reduce health inequities this much.
Why is a tobacco endgame so powerful at reducing Māori and non-Māori health inequities? Because smoking is so bad for health, smoking rates are particularly high among Māori, and Māori also have higher smoking-related disease rates.
Therefore, Māori see more health gains from the dramatic falls in tobacco smoking that will result from the policy. (Non-Māori also see large gains – just not as much per capita as Māori.)
What about overall health gains? Our modelling suggests that, over the remaining lifespan of the New Zealand population alive in 2020, the tobacco endgame strategy will result in an extra 600,000 “health-adjusted life years” lived (a measure of the impact of those interventions on life expectancy, adjusted for quality of life).
To put this in perspective, this amount of health gain – accruing just to those people quitting smoking earlier or not taking it up, a minority of the population – is equivalent to the health gains that would result from a policy taxing sugar, fat and salt in all foods and removing the GST on healthy food.
Read more: How can we reverse the vaping crisis among young Australians? Enforce the rules
Major health system savings
Not only is this endgame policy increasing the health of the nation, it is also reducing future health expenditure.
We estimated NZ$1.3 billion of health system costs would be avoided in the next 20 years. These savings can be used for other things, such as mental health and dementia care.
And while the government will lose tax revenue from drastically reduced tobacco sales, the overall health of the population increases, meaning more people are in work for longer. We estimated an income gain to the New Zealand population of $1.4 billion in the next 20 years, which means more tax revenue as well.
All modelling of the future is uncertain. But even allowing for that uncertainty, the health gains, the health inequity reductions, the savings in health expenditure, and the increased income productivity of New Zealanders that will result from this tobacco endgame strategy will be large.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.