Doctors are hailing a “remarkable” new treatment regime for cervical cancer that reduces the risk of dying by 40%, in the biggest advance against the disease in 25 years.
Cervical cancer is the fourth most common cancer in women globally, with about 660,000 new cases and 350,000 deaths every year, according to the World Health Organization. In the UK, there are about 3,200 cases and 800 deaths each year.
Many of those affected are in their 30s, and despite improvements in care, the cancer returns in as many as 30% of cases.
The new treatment plan was tested in patients recruited over 10 years from the UK, Mexico, India, Italy and Brazil. It involves a short course of chemotherapy before patients undergo chemoradiation, the standard treatment for cervical cancer involving a combination of chemotherapy and radiotherapy.
In research led by University College London, it has been reported that the results of the phase-three clinical trial showed a 40% reduction in the risk of death from the disease and a 35% reduction in the risk of cancer coming back within at least five years. Their findings have been published in the Lancet.
Dr Mary McCormack, the lead investigator of the trial at UCL, told the Guardian the discovery was the most significant breakthrough in treating cervical cancer since the end of the last century. “This is the biggest gain in survival since the adoption of chemoradiation in 1999,” she said.
“Every improvement in survival for a cancer patient is important, especially when the treatment is well-tolerated and given for a relatively short time, allowing women to get back to their normal lives relatively quickly.”
Researchers at UCL and University College London hospital (UCLH) completed a long-term follow-up of patients who were given the short course of chemotherapy before chemoradiation.
The Interlace trial, funded by Cancer Research UK and UCL Cancer Trials Centre, looked at whether a short course of induction chemotherapy prior to chemoradiation could cut relapses and deaths among patients with locally advanced cervical cancer that had not spread to other organs.
The trial recruited 500 women who were randomly allocated to receive either the new treatment regime or the standard chemoradiation treatment. None of the patients’ tumours had spread to other organs.
In the study, one group received the new regime of six weeks of carboplatin and paclitaxel chemotherapy. This was followed by standard radiotherapy plus weekly cisplatin and brachytherapy chemotherapy, known as chemoradiation. The control group received only the usual chemoradiation.
After five years, 80% of those who received a short course of chemotherapy first were alive and for 72% their cancer had not returned nor spread. In the standard treatment group, 72% were alive and 64% had not had their cancer return or spread.
Separately, UCL said the trial found a 40% reduction in the risk of death and a 35% reduction in the risk of cancer returning, when comparing the two groups using a different metric.
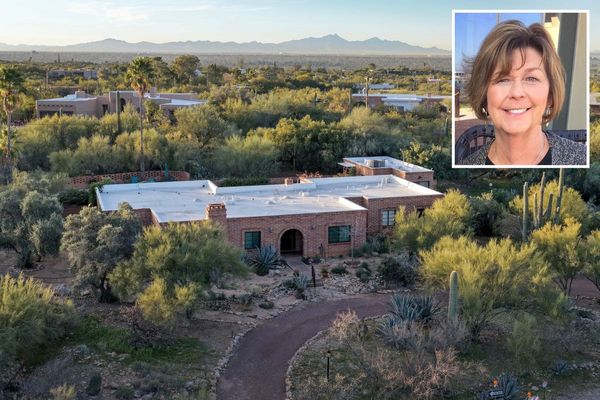
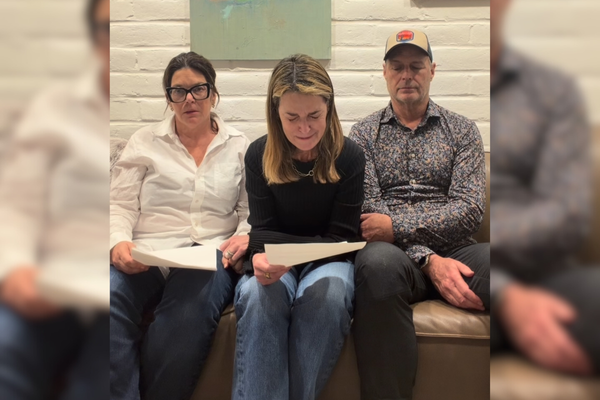
Abbie Halls, a client service manager from London who was diagnosed with cervical cancer when she was 27, is one of the women who received the new treatment regime. “I’ve been cancer-free for over nine years now and I’m not sure if I’d be here without the treatment that I received,” said the 37-year-old. “I’m happy that I could play a part in advancing the research, which I hope is going to save the lives of many more women in years to come.”
The results prompted calls for the regime to be implemented across the UK and internationally. McCormack said: “A short course of induction chemotherapy prior to standard chemoradiation treatment greatly boosts overall survival and reduces the risk of relapse in patients with locally advanced cervical cancer.
“This approach is a straightforward way to make a positive difference, using existing drugs that are cheap and already approved for use in patients. It has already been adopted by some cancer centres and there’s no reason that this shouldn’t be offered to all patients undergoing chemoradiation for this cancer.”
Dr Iain Foulkes, the executive director of research and innovation at Cancer Research UK, said: “The simple act of adding induction chemotherapy to the start of chemoradiation treatment for cervical cancer has delivered remarkable results. A growing body of evidence is showing that additional chemotherapy before other treatments, like surgery and radiotherapy, can improve the chances of successful treatment for patients. Not only can it reduce the chances of cancer coming back, it can also be delivered quickly, using drugs already available worldwide.”