A mum-of-two died after a tube that was helping her breathe came loose after life-saving surgery, an inquest heard. It has led to a hospital trust implementing new procedures and training in an effort to prevent it happening again.
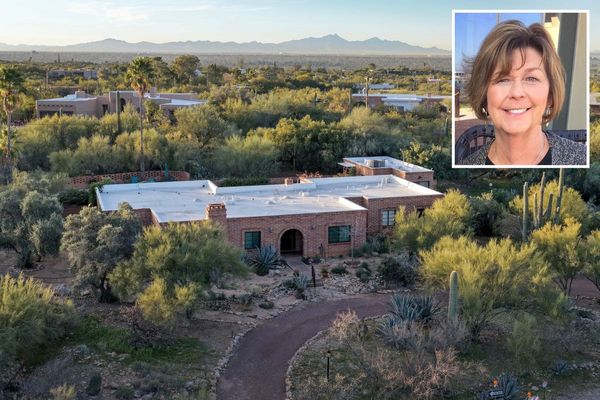
Melanie Coops, 50, was taken to Wythenshawe hospital on February 25 last year after contracting Covid during the height of the second wave of the pandemic. The mum was then put on a ventilator three days later to help her condition of pneumonitis which was badly affecting her lungs. The ventilator did improve her condition over the proceeding weeks.
Her condition improved to the point that doctors attempted to take her off the ventilator so she could breathe herself. However, within an hour of this Melanie 'rapidly deteriorated' and had a cardiac arrest.
Staff were able to stabilise her and get her ventilated again. But it was decided she would need a tracheostomy - an opening created at the front of the neck so a tube can be inserted into the windpipe (trachea) to help breathing.
After this it was discovered that the Covid and lack of oxygen her organs were getting as a result of the virus had resulted in her developing bowel ischemia, which could have proved fatal if left untreated. An operation to address this took place on March 17, which is where many more problems occurred, an inquest at Manchester Coroners Court heard last week.
The major operation itself went well, according to consultant anaesthetist at Wythenshawe Hospital, Dr Alex Bojarksa, who was present at the operation. However, there was a 'crisis' when Melanie was moved from the operating table to the hospital bed.
At some point during the moving of the bed, the tracheostomy tube, which was supplying Melanie with oxygen, dislodged so she was no longer receiving oxygen. Due to her overall health, including a high BMI and asthma, and the severe Covid infection, Melanie quickly went into cardiac arrest, and Dr Bojarksa and other doctors had to make split second decisions to try and save her.
"That's when all the action started," Dr Bojarksa said. "This is a very dramatic situation with a patient like this who is extremely sick.
"The situation suddenly went from very controlled to very dramatic. We tried to insert a tube through her mouth so she could breathe again. There were three different attempts at this to try and make it work.
"We knew we had very little time to do this, we knew she would quickly go into cardiac arrest due to having nearly no oxygen reserves."
Melanie went into cardiac arrest within 60 seconds while the doctors continued to try and ventilate her. She was ventilated but had suffered catastrophic brain injuries in this time, despite it being very short.
"Every second counted so much," Dr Bojarksa added. "Time was such a critical factor here and we were going through all of our processes and steps as fast as possible."

Melanie's high BMI, severe Covid infection, pneumonia, bowel operation, the tracheostomy tube dislodging, the difficulty in accessing her airways in those split seconds, and quick cardiac arrest were just some of the factors making this an incredibly difficult and complex situation for the doctors. Other factors including the heavy PPE they were wearing at the time, the incident occurring at the end of a 12-hour shift for the staff, also made this more difficult Dr Bojarksa said.
"All of these factors came together at the same time in this tragic way, so many things went wrong all at once. We have processes to avoid panic and stress but everything happened so quickly."
Dr Nick Wisely, a consultant anaesthetist at Wythenshawe Hospital, started an investigation the day after this incident and reiterated the complex nature of this case. Dr Wisely and senior anaesthetist Dr Brendan McGrath who specialises in patient safety around tracheostomies made an investigation report after this incident to see how Manchester University Foundation Trust could improve after this.
"This was an incredibly significant incident as lots of things were all happening together," Dr Wisely told the inquest. "We immediately learned from the incident, to reduce the chance of this happening again."
He described how Melanie 'took a turn for the worse' on March 15 and her bowel problem deteriorated more over the next few days. After the operation staff noticed she was no longer being ventilated and she "incredibly quickly had a cardiac arrest".
"She had no oxygen reserves so any dip in ventilation would cause a cardiac arrest within seconds," he added. "It was astonishing how many contributing factors there were at the same time."
Senior Coroner Nigel Meadows commented that it became the 'perfect storm' of all these factors coming together at the same time, leading to Melanie's rapidly deteriorating state.

Dr Wisely added that with during this time, at the height of the Covid pandemic, only essential equipment and staff were in theatres at any one time. This meant that some equipment that would usually be in the theatre to help reopen a person's airways in this type of situation were not.
This, along with the heavy PPE they were wearing, an 'obstacle course' of an operating theatre, shift changes taking place at this moment meaning there were more people in the theatre than normal, caused the 'perfect storm' for Melanie, Dr Wisely said.
Dr Wisely met the next day with staff to discuss if that there were any 'immediate steps' that needed to be taken to learn from this incident. He pointed out that strict Covid protocols are not in place anymore, so they are not 'cucooned' in PPE.
"Straight away we recognised that we needed to look further at what was going on with tracheostomies," Dr Wisely said. "We realised the need for further education to improve training and simulations around tracheostomies."
A project group was set up at MFT to look at the common problems arising from tracheostomy incidents and how staff could be educated to deal with these. He said: "The key things done are to speak to colleagues about the incident so people can see what happened and the different factors that were involved to highlight the different areas of the tracheostomy to draw attention to the guidelines around it that are widely available."
At MFT there is a simulation of this situation that is a 'core part' of training around tracheostomies now. "There are some positive lessons from these tragic events but it won't bring her back unfortunately," Dr Wisely said.
However, it was added that even if the tracheostomy had not come loose, triggering the cardiac arrest, Melanie's health was so poor from the Covid that she had less than a 50 per cent chance of survival. "But we won't know," Dr Wisely said.
The family asked Dr Wisely if these training simulations had been useful since Melanie's death for MFT, and if this should be implemented nationwide. He said: "Locally we have benefited from the simulations, I'm sure there are other trusts that do it do, but we have certainly benefited and think it should be done everywhere."
In a gofundme fundraiser towards Melanie's funeral costs, her husband Craig said: "Melanie was a loving wife and mother who loved horses and dogs and animals."
A spokesperson for Manchester University NHS Foundation Trust added: “We wish to express again our sincerest condolences to Melanie’s family. We are committed to learning from this tragic incident, and we have already made improvements to our systems since then to make our practices safer.”
Get the latest headlines and more sent to your inbox by signing up to our free newsletter here.