
Overwhelmed hospitals are putting A&E patients alongside women on maternity wards and cancelling hundreds of cancer operations in a bid to deal with the worst ever crisis in emergency care.
An investigation by The Independent has revealed an alarming escalation of the NHS crisis in all areas of the health service as new figures released on Thursday showed 54,532 patients waited 12 hours for an A&E admission in December, a monthly rise of 44.1 per cent.
As ambulance waits reached an average of 90 minutes for strokes and heart attacks, one patient described a Cardiff A&E as “mayhem” with no free spaces, people lying on the floor with oxygen tanks and queuing in hallways. The Independent also found:
- An 82-year-old man with chronic kidney disease waited 56 hours on a trolley in a corridor before being admitted for treatment
- An 89-year-old cancer patient slept in a corridor dubbed “the A&E patient car park” and waited 46 hours for a scan
- A consultant at a major hospital said they were cancelling operations “left, right and centre” and the intensive care unit was “absolutely rammed”.
Dr Simon Walsh, of doctors’ union the British Medical Association, said the health service was “in unprecedented territory, where harm is actually occurring week after week”. He added: “The situation now is far worse than I’ve ever experienced. We’ve never really thought that any government would let it get as bad as it is now.
If you have an A&E story to share, email Rebecca.Thomas@independent.co.uk
“The thing that’s new is being in an environment where you feel unable to deliver safe care to even those with the highest need. It’s soul-destroying."
‘Standing room only’
Frank Newton, an 82-year-old with stage four chronic kidney disease, was rushed to Whiston Hospital near Liverpool by his daughter Andrea Newton on 28 December with suspected pneumonia. They had been told by their GP the wait for an ambulance would be 30 hours.

What followed, she says, was a “living nightmare” as they waited 56 hours on a trolley in a holding area. “One night I counted 19 ambulances outside the hospital, around 40 to 50 people in the corridors and maybe another 50 or more in the waiting room where it was literally standing room only,” Ms Newton said.
As her father writhed in pain and became increasingly delirious, Ms Newton sought help, only to be told he was “just one of 50 patients”.
Last month 2.2 million patients sought help at A&E, but only half of them were seen within the target of four hours. Earlier this week, we revealed the number waiting more than 12 hours had exceeded 50,000 for the first time.
The Commons health select committee announced it would investigate the link between excess deaths and long A&E waits after The Independent reported calculations showing delays could be contributing to 500 deaths a week.
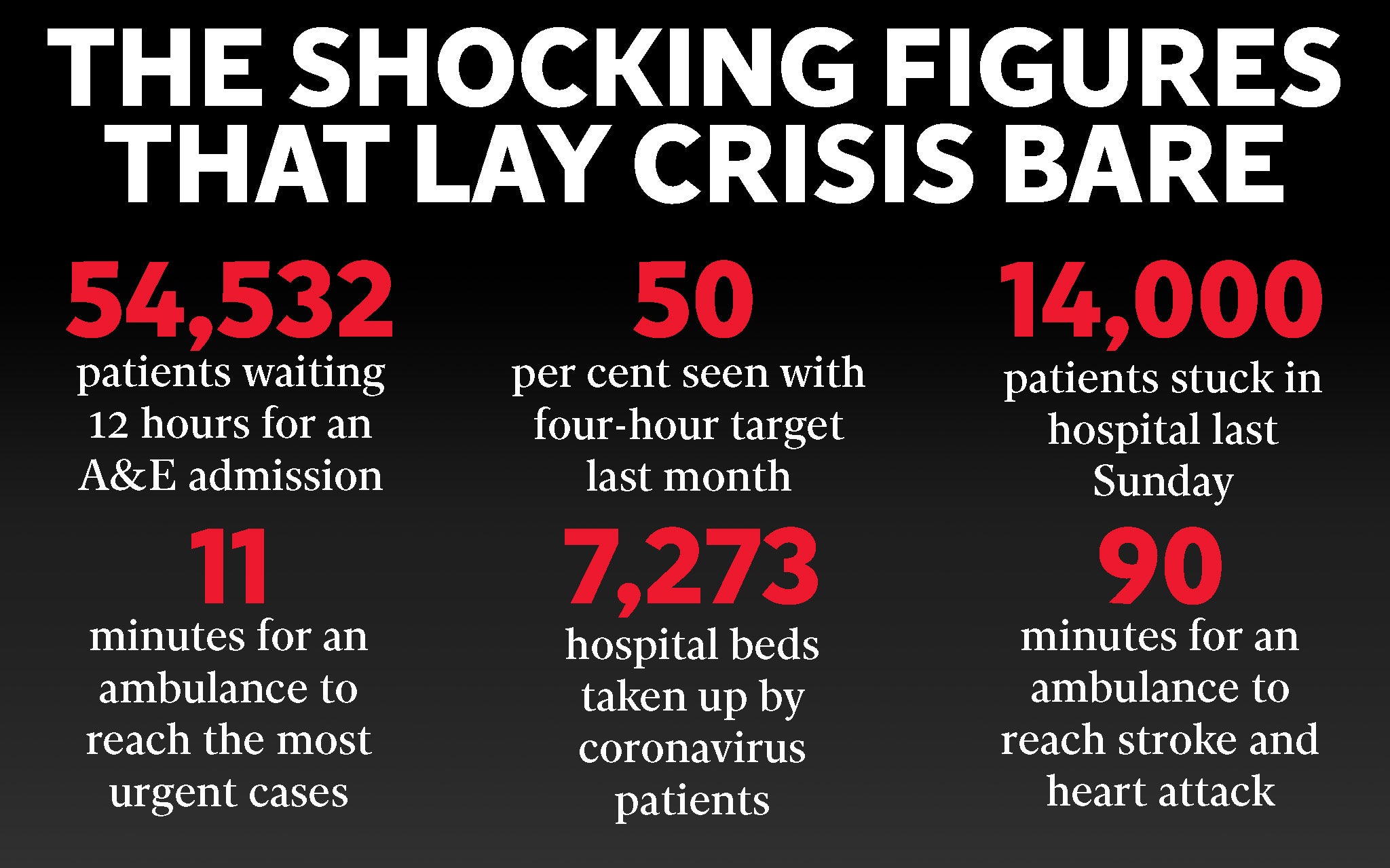
Ambulance delays were also the worst on record, as the average response for the most urgent incidents, such as cardiac arrest, dropped to 10 minutes and 57 seconds – almost four minutes higher than the target. For category two emergencies, such as strokes, they took an average of an hour and a half to respond, compared with a target of 18 minutes.
Tom Johnson, a cardiologist in Bristol, said over Christmas one of his patients with chest pain was told no ambulances were available and his family had to drive him to hospital. He suffered cardiac arrest en route and, without a paramedic to offer treatment, he died. Dr Johnson said: “The system needs to change to save that man’s life. We are unable to provide the care we want despite our best efforts.”
The prime minister’s official spokesperson said the delays were “obviously not acceptable”.
‘It was like a war zone’
John Syers, 89, was taken to William Harvey Hospital in Ashford, Kent, shortly before Christmas after doctors suspected he had a tumour on his spine. Mr Syers, who is being treated for cancer, should have been taken to a ward while he waited for an emergency MRI scan.

Instead, he was put on a bed in a corridor that Mr Syers’ son, Paul Syers, says was referred to as the “A&E patient car park”. His son said: “He was distressed, seven metres away from a door that’s constantly opening and closing. He had no sleep all night. It was like a war zone, it was terrible.”
The next day he was moved to another corridor, before finally having a scan 46 hours after arriving.
The overcrowding in emergency departments is forcing patients who are immunocompromised, and so cannot risk picking up infections, to take desperate measures in order to be seen by doctors.
Diana Isajeva, who is waiting for a life-saving kidney transplant, went to Heath hospital in Cardiff on 29 December suffering suspected shingles. She said: “[A&E] was honestly mayhem. There were no free spaces. No free seats anywhere. The whole waiting room was full of very seriously ill people. People were on the floor with oxygen tanks. There were people queuing up in the hallways - all the hallways were full of people on the trolleys. Nobody was wearing any masks, there was no Covid safety and no flu safety.”
Immunocompromised patients should be immediately moved to an area where the risk of infection can be controlled, such as a ward. But with no spaces available, Ms Isajeva instead had to wait in her car for 14 hours before a doctor became available. She said: “It was freezing cold on that day. I couldn’t go to the toilet inside the hospital because there is no network [coverage] inside the hospital so, if anybody called me on my phone to come and see the doctor, they weren’t able to reach me. I had to go in the nearby bushes for the whole 14 hours.”
‘Overwhelmed with demand’
In an email to staff this week, Foluke Ajayi, chief executive of Airedale NHS Foundation Trust, which runs a district general hospital in West Yorkshire, said: “In all my years in the NHS I have never seen such a challenging Christmas/New Year period as this one. This was the first time I’ve seen all of us in West Yorkshire – and nationally – overwhelmed with demand, with such acutely unwell patients.”
The director of a hospital trust in London told The Independent the waits over Christmas had been an “eye-watering” average of 22 hours, with beds for adults squeezed into paediatric surgery wards, while female surgical patients were treated in the maternity day unit. They added: “This was necessary but has a huge impact on patient experience and the quality of care we can deliver.”

As the push for space to treat emergencies grows, cancer surgeries are among those being cancelled. A consultant at a hospital in Coventry said: “We are cancelling operations left, right and centre. It is extremely frustrating seeing theatre teams who are unable to do anything because there are no beds for the patients we need to operate on. They said their hospital’s intensive care unit was “absolutely rammed”, adding: “We are opening up a surge area and we just don’t have enough staff for it.” Another senior doctor, in Nottingham, said the cancellation of cancer surgery was continuing even though their hospital no longer had an active “critical incident”.
‘Provide care yourself or pay for it’
The surge in demand at A&E last month has been attributed to a resurgence of Covid, with 7,273 beds taken up by coronavirus patients, and a spike in flu. For NHS 111, calls ramped up from 58,000 in November to 95,000. Professor Sir Stephen Powis, NHS England’s national medical director, said on Thursday that this “twindemic” had led to “unprecedented levels of respiratory illness in hospital”.
“Bed blocking” is also increasingly taking up resources because of a lack of appropriate care in the community. NHS data shows the number of patients delayed in hospital passed 14,000 for the first time last Sunday.
This comes against a backdrop of strikes across the NHS, with 25,000 ambulance workers walking out on Wednesday for the second time in less than a month. NHS directors across the country told The Independent that, although demand was manageable on the day of the strike itself, they fear a “rebound effect” will increase patient numbers in the coming days.
On Thursday, the Commons health select committee launched a probe into the link between excess deaths and A&E delays. It comes after The Independent revealed 500 excess deaths a week could be linked to long trolley waits.
There are also fears that a lack of appropriate care means discharged patients are being taken to emergency departments. Dr Dave Triska, a GP in Witley, Surrey, said: “The main issue at the moment is people are arriving home from hospital in a semi-collapsed state, with next to no care arranged through lack of services. Inevitably there is a rapid deterioration and re-admission. This is now common.
“The amount [of people to whom] I now say, ‘I’m sorry this is as good as it gets, either you’ll have to provide care yourselves or pay for it,’ has increased dramatically. It’s now common, and the looks from families are haunting – they think there is a safety net there. There isn’t any more.”







