For anyone trying to lose weight, there’s a truth we can all universally acknowledge: Numbers aren’t fun. From the digits on a scale to the body mass index in your medical records, better health is often positioned as a numbers game — especially for people whose weight means they are categorized as obese according to the BMI. Hit the right number, and all your health problems will magically resolve, so the logic goes.
Yet increasingly, science is revealing that measures like the BMI are misleading — and that losing weight may not be a silver bullet after all. That’s the takeaway from a new paper in the journal Science that finds weight loss may come with unexpected — and not entirely desirable — health effects.
What’s new — In a mouse study published Thursday in the journal Science, researchers found that inflammation lingered in mice that had been fed a high-fat diet after the rodents shed the ounces. The findings hint at a potential mechanism for the seeming link between obesity and inflammation, as well as evidence that these issues may remain regardless of whether or not one loses weight.
“[The paper] asks a question that goes beyond what a lot of us are asking right now, which is… if you reverse obesity and lose the weight, what are the effects? Do the mostly negative effects of obesity persist or continue to exist?” Sagar Bapat, an assistant professor at the University of California San Franciso’s Diabetes Center and the Department of Laboratory Medicine, tells Inverse. Bapat was not involved in the study.
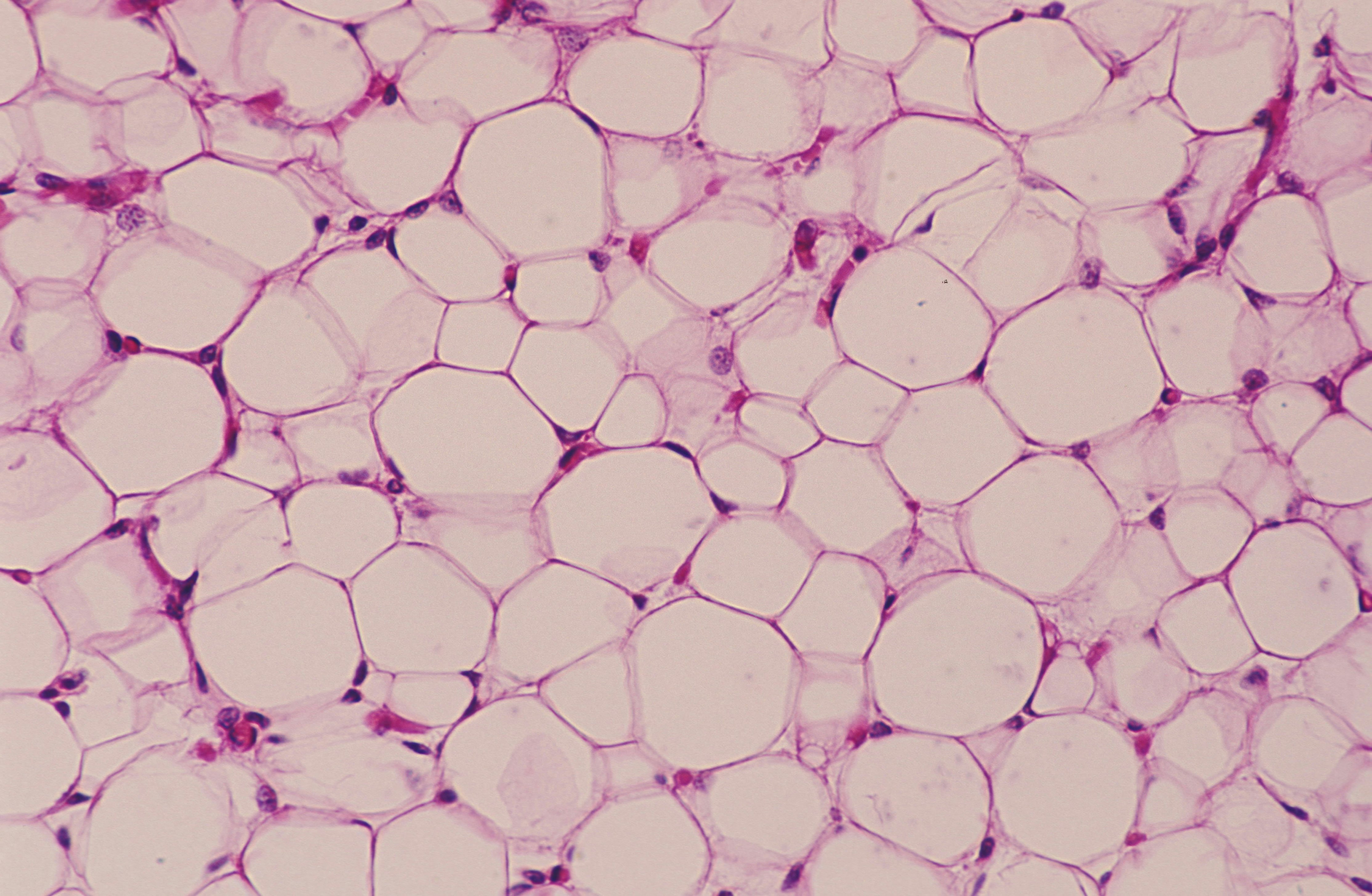
Looking specifically at an inflammatory eye condition previously linked to obesity called age-related macular degeneration, mice fed a high-fat diet appeared to undergo a change in the genetic code of immune cells called macrophages. While the mice returned to a typical weight and metabolic state, their immune cells remained changed — and the inflammation stuck around, too.
Here’s the background — Scientists have spent years trying to tease out the links between weight, metabolism, and the immune system. In a typical body, adipose tissue (fat) acts as an energy storage facility, stocking up surplus nutrients for when times food is scarce. Fat is ordinarily full of immune cells; when body conditions are hunky dory, these cells do the job of protecting the body and keeping inflammation at bay.
The problems start when there’s too much stockpiling. Individual fat cells (adipocytes) grow larger and expand. Over time, these overwhelmed and stressed cells start releasing hormones and chemicals that encourage what’s called chronic low-grade inflammation.
This simmering stressful state inflicts structural damage onto adipose tissue itself and organs like the heart and eyes. Immune reactions triggered by chronic low-grade inflammation can, in turn, help spur conditions like cancer and diabetes and put individuals at a greater risk of contracting infectious diseases like Covid-19. In the case of age-related macular degeneration, inflammation of the retina causes irreversible blindness. Being within the criteria for obesity according to the BMI is a known risk factor for the condition, but how chronic low-grade inflammation influences the disease isn’t well studied. Nor is the theory that simply losing weight — and dropping out of the obese category on the BMI scale — might have a protective effect.
How they did it — To try and answer this question, the researchers conducted several experiments on young mice that were fed a high-fat diet — about 60 percent fat — for 11 weeks, which made them gain weight. The mice were then put on a diet of low-fat food — 10 percent fat — for nine weeks, which made them lose weight. Another group of mice only ate the low-fat diet as a control.
The researchers then shot lasers into the eyes of both the yo-yo dieter mice and the control mice to encourage atypical blood vessel growth, which is a hallmark of age-related macular degeneration. After another two weeks, the researchers examined the mice’s body tissues in detail for any immune cell changes.
Separately, the researchers also took fat from the bellies of formerly plump mice, transplanting the tissue into average-weight mice. These mice also underwent the same laser-in-the-eyes procedure some weeks after their fat transplant surgery to see if the fat tissue itself had any effect. Spoiler: It did.
What they found — Among the mice that had gained and then lost weight, there was about 40 percent more atypical blood vessel growth than their stable diet peers.

Driving the growth appeared to be a type of immune cell called a macrophage, a white blood cell that promotes healing after injury. But in the yo-yo dieter mice, these cells had been reprogrammed to cause inflammation, not healing. The reprogrammed cells were also present in the typical-weight mice which had had fat tissue transplants. Taken together, these cells appeared to have an outsize role in atypical blood vessel growth in the eyes.
By digging further into the genetic code of the macrophages, the researchers found a link between the high-fat diet — specifically stearic acid, a saturated fat —and epigenetic changes. These are modifications that turn on or off certain genes — in this case, those to do with inflammation. Meanwhile, in the mice fed only a low-fat diet, these inflammatory changes were absent. The results suggest that eating a high-fat diet that causes weight gain, even if followed by weight loss, leaves an inflammatory mark on mouse macrophages.
Why it matters — Obesity is considered a risk factor for myriad health conditions, but the mechanisms are not well-studied. In turn, the go-to remedy — that someone considered obese and at risk of inflammation-related health problems should just lose weight — is also not well-studied, despite being widely accepted as established fact.
“There are projections that one out of every two American adults will be obese by 2030,” says Bapat.
For some people, losing weight can come with immense health benefits, such as reduced blood pressure and cholesterol, as well as a lower risk for metabolic disease. But this study suggests the struggle for better health doesn’t necessarily end with weight loss.
What’s next — The study does not reveal whether the epigenetic changes last for weeks, months, or years, and nor does it account for the fact that epigenetic changes in a parent resulting from diet or stress can be passed onto their child. And, because the study is in mice, it is an open question whether the results would hold true for humans, although shared biology with mice do make it likely, Bapat says. More research is needed to tease out the nature of this complex relationship.
In the broader social context, the research comes during a period of renewed interest in anti-obesity drugs. For example, pharma companies tout breakthrough anti-obesity drugs, such as Novo Nordisk’s Wegovy and Eli Lilly’s tirzepatide. But medications that help people shed pounds do not also treat or prevent inflammation linked to a history of a high-fat diet and weight gain.
“The question of how to actually engage [these findings] with pharmacological interventions is perhaps, right now, the challenge,” says Bapat, who’s done research in his own lab at UCSF looking at T cells (another immune cell) in obesity.
“I think we’ll probably, over time, find strategies that are actually tractable in human beings,” he adds.