It is the 60th anniversary of Medicare, but no one seems to care.
It is, after all, hard to be enthusiastic about a system in crisis. Patients can’t find doctors (almost one in five Canadian adults). Those who have doctors have a hard time getting in to see them (only 18 per cent can get an appointment within a day or two).
Doctors are burned out, leaving their practices with no one to replace them. New physicians want to focus on patient care, not the business of health care.
This is, of course, just the beginning of the problem. The premiers want more money from Ottawa and Ottawa wants more data from the provinces. Alberta is making health proposals that some say are a short step away from privatized health care, and the recent meeting between federal and provincial health ministers ended in a stalemate.
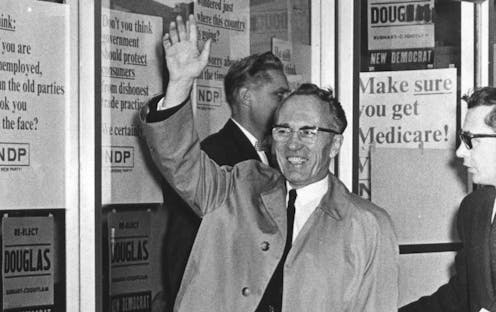
The dawn of Medicare

These seem like intractable problems. But our research suggests part of the solution might be found back in 1962, when the model that would grow into our current health-care system was launched in Saskatchewan, spreading to other provinces over the next few years.
At the dawn of Medicare, the proposed new model resulted in a strike by Saskatchewan doctors worried about “socialized medicine.”
Faced with the prospect of losing access to their doctors, almost 15,000 families (representing 50,000 people) formed 34 community clinic associations, raising over $325,000 (almost $3 million today) over less than a year for health-care clinics that patients would own and govern based on democratic co-operative principles.
The clinics adopted a philosophy of care that rejected many of the tenets of conventional medicine, which Stan Rands, a clinic organizer, described as focused on “physiological and biochemical causes of disease” and dependence on “equipment and tests for the diagnosis and treatment of illness.” The result, he argued, was that it was “ill-equipped to deal with the human and social manifestations of illness or disease.”
The community co-operative clinic model
Based on this philosophy, the clinics implemented what were, at the time, radical measures. Instead of being paid on a fee-for-service basis, doctors were paid salaries. Instead of sole practitioner businesses, doctors worked as part of a team deeply engaged and responsive to their communities because the clinics were run by patients. Instead of treating symptoms, the team treated patients holistically, probing the physical and social factors that we now know lead to illness.
Although the clinics strengthened the government’s hand in reaching a settlement with the striking doctors, the province never embraced the co-operative clinic model. Instead, the clinics would spend years struggling to be understood by policymakers who tended to favour a conventional system based on fee-for-service, doctor-led Medicare.

Many clinics folded shortly after Medicare was introduced; today, only four remain, with large clinics in Saskatoon, Regina and Prince Albert, and one smaller rural clinic operating in Wynyard. Even the 2002 Commission on the Future of Health Care in Canada, led by former NDP premier of Saskatchewan Roy Romanow, ignored the sector’s efforts to put its model on the agenda.
Away from the spotlight, the remaining co-operative clinics went about living their philosophy. They hired social workers, offered mental health services, brought in physiotherapists, set up pharmacies, offered in-house minor surgeries, performed house calls, operated forerunners to modern-day telehealth, and set up shop in disadvantaged, poorly served communities like Saskatoon’s west side.
The future of co-op clinics
Meanwhile, there are signs that the philosophy of team-based, patient-focused, community-based care may be gaining ground. In 2017, for example, Ontario’s Matawa First Nation opened the country’s first Indigenous-run co-operative clinic.
The provincial government in Ontario operates a large network of not-for-profit community clinics similar in structure to Saskatchewan’s clinics but lacking explicit democratic co-operative control. In addition, some Canadian doctors are now advocating for a different model.
À lire aussi : The doctor won't see you now: Why access to care is in critical condition
Elsewhere, there are indications that citizens may be tired of waiting for policymakers to act. As the Globe and Mail recently reported, residents of the Saanich Peninsula, on the southeast coast of Vancouver Island, raised money to open two medical clinics and recruit doctors who could take over from physicians at, or near, retirement. As Dale Henley, the co-chair of the non-profit that owns and operates the clinics told the Globe and Mail,
“I think we’ve got to do a little more ourselves. We can’t just keep looking at governments all the time, because they’re not that good at it.”
As we look back on 60 years of Medicare and contemplate its many challenges, it may be time for communities to heed Henley’s call and once again voice their desire in words and action for access to the kind of holistic care pioneered by the co-operative clinics. Maybe this time, policymakers will listen.
Marc-Andre Pigeon is the director of the Canadian Centre for the Study of Co-operatives. It receives funding from the co-operative and credit union sector. The research into the co-operative clinics is funded, in part, by the Saskatoon Community Clinic, one of the clinics being investigated in this research.
Natalie Kallio is a Professional Research Associate at the Canadian Centre for the Study of Co-operatives, which receives funding from the co-operative and credit union sector. This research is funded, in part, by the Saskatoon Community Clinic, one of the clinics being studied.
Haizhen Mou ne travaille pas, ne conseille pas, ne possède pas de parts, ne reçoit pas de fonds d'une organisation qui pourrait tirer profit de cet article, et n'a déclaré aucune autre affiliation que son organisme de recherche.
This article was originally published on The Conversation. Read the original article.







