A LEADING doctor has described the situation for Scotland’s GPs as “dire” and warned that the country is “sleepwalking towards a two-tier health service”.
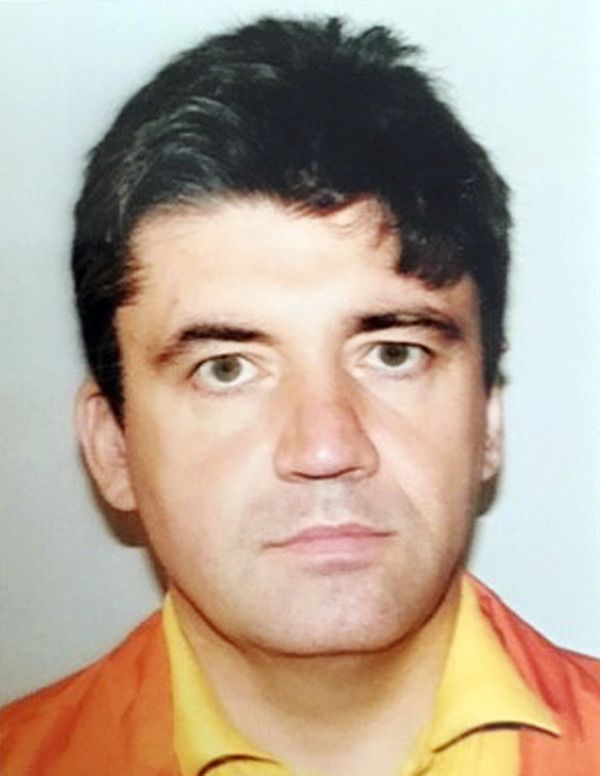
Dr Andrew Buist, the chair of the British Medical Association’s Scottish general practice committee, said that the new first minister must show a “greater commitment to actually delivering” for GPs.
In a blog post published on the BMA website, he added that without action to address the issues faced by family doctors, Scotland could see the emergence of “under-doctored areas” – where a lack of GPs makes it difficult for patients to register with a practice.
Such a situation could lead to “increased levels of health inequalities” in Scotland, he warned, as well as creating opportunities for private GP services.
Buist also told how GPs were “demoralised”, saying that they have to deal with a "mismatch" between demand and capacity every day.
Rather than an increase in the number of GPs, as promised when the BMA developed the Scottish GP contract with the Scottish Government, Dr Buist said the whole time equivalent (WTE) number of GPs “is actually falling” – saying in some areas this meant there were more than 2000 patients for every GP.
The GP contract had been designed to set out a “new direction for general practice in Scotland”, but Dr Buist claimed that “it seems we lost our political commitment to this project”.
Calling for action from the new first minister, who will take office next week, he insisted action was needed “beyond some of the warm words we often hear, but are wearing exceptionally thin at this tipping point”.
Health Secretary Humza Yousaf is one of three candidates running to replace Nicola Sturgeon as Scottish first minister, going up against Finance Secretary Kate Forbes and former community safety minister Ash Regan for the top job in Scottish politics.
But Dr Buist told them: "In short, the present situation is dire and is only going to get worse without intervention."
He said: “We must look with hope to the new first minister and (potentially!) new Cabinet secretary for health to show greater commitment to actually delivering for general practice and recognise it as the foundation of our NHS in Scotland.”
While Scottish Government figures showed an average of 26,331 people attended accident and emergency each week in January this year, he said this total compared to the average of 703,310 direct patients contacts each week in general practice over the course of 2022.
Dr Buist said this level of activity meant any loss of GP practices would “inevitably impact on the rest of the NHS system”.
And he said that ministers “need to understand that when general practice fails, the NHS will surely fail”.
Speaking out about the situation GPs are facing, he said: “Most days are now just about survival and dealing with the acute situation.”
Dr Buist said that “almost no practice can consider themselves immune to the recruitment and retention problems that could force them to give up their contract”.
He said there had been a failure to create new practices “in those areas of Scotland witnessing population expansion due to a local house building boom”.
And he added: “We have failed to invest in the GP premises estate such that many are in a very poor state of repair and are inadequate to meet the needs of modern patient care.”
Dr Buist said “despite everything” the BMA in Scotland still believed in the GP contract, describing it as being the “keystone development for NHS reform of patient care in Scotland”.
But he insisted: “It requires vision, a resolve to deliver and significant investment if it is to be achieved.”
Dr Buist said: “The alternative is the path we have recently been unwittingly led on, sleepwalking towards a two-tier health service.
“A direction that will see a continued loss of GPs, with practice contracts given back to their health board, the subsequent closure of some practices, and an emergence of under-doctored areas where patients have difficulty registering with a GP.”
A Scottish Government spokesperson said: “The Scottish Government is fully committed to the 2018 GP contract, supported by over £170 million of investment this financial year alone, and over £500 million since its inception.
“We have continued to implement the new contract throughout the worst of the pandemic, recruiting over 3220 additional healthcare professionals who are working alongside GPs and practice teams, ensuring patients see the right person at the right time for their healthcare needs.”