In 2011, the Indian government introduced the H1 rule to prohibit the over-the-counter (OTC) sales of antibiotics without a prescription, responding to the growing concern over antimicrobial resistance (AMR). However, due to the healthcare system’s heterogeneity across the country, the implementation of this rule faced significant challenges. In 2013, following the Chennai Declaration document and initiative by medical societies in India, the Indian government modified the rule to limit the OTC restriction to second- and third-line antibiotics, allowing the sale of first-line antibiotics without a prescription. This modification was aimed to ensure that life-saving antibiotics remained accessible to the public, especially in remote areas of the country where doctors might not be readily available. Despite a decade passing since the rule’s announcement, no State government had adopted it until Kerala recently initiated Operation AMRITH (Antimicrobial Resistance Intervention for Total Health). This programme enforces the original H1 rule, mandating a doctor’s prescription for acquiring any class of antibiotics.
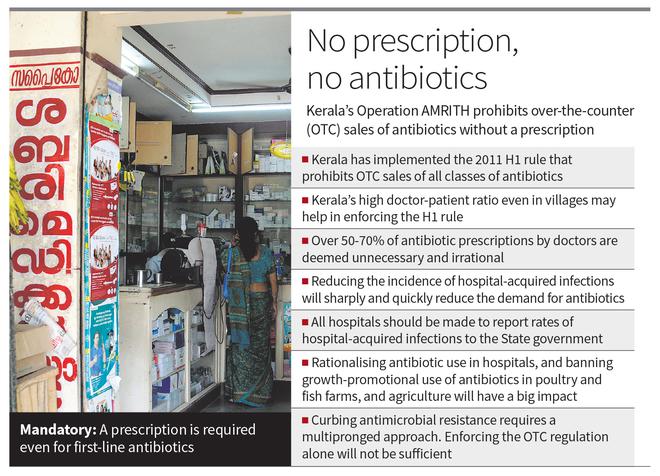
Kerala’s high doctor-patient ratio, even in villages, facilitates the enforcement of this rule. Also, the high literacy rate in the State is poised to contribute significantly to the efficient implementation of the rule. An informed populace is more likely to understand the importance of regulations like these and adhere to them, facilitating smoother execution and compliance. While it is highly commendable that Kerala is implementing the H1 rule to rein in AMR, it is unlikely to have a significant impact on drug-resistant infections in the immediate future. The effects of this initiative may take several years, if not a decade, to manifest. However, it will foster a culture of respecting antibiotics and encourage further actions to combat AMR.
It is critical to acknowledge that over 50-70% of antibiotic prescriptions by doctors are deemed unnecessary and irrational. One of the main reasons for unnecessary antibiotic usage is the unavailability of laboratory facilities to make a correct diagnosis of bacterial infections. Even if they are available, these tests are more expensive than a course of antibiotics. Enhancing laboratory facilities for accurate infection diagnosis, especially with affordable rapid diagnostic tests to determine the necessity of antibiotics, is therefore vital. The other main reason for unnecessary antibiotic prescriptions by doctors is the pressure from patients to receive antibiotics; patients wrongly believe that a course of antibiotics is a quick remedy for a fever episode of any cause. Educating patients about the limitations of antibiotics and discouraging them from pressuring doctors for unnecessary prescriptions is vital.
While it is commendable that the OTC regulation without a prescription has been put into place, what is even more important is that Kerala demand hospitals to disclose the incidence of hospital-acquired infections. Antimicrobial resistance is a socioeconomic problem, and combating it requires measures to improve public health infrastructure, sanitation facilities, and governance in order to decrease the transmission of infections and, therefore, the dependence on antibiotics. The influence of these factors on antimicrobial resistance rates is typically greater than that of the total volume of antibiotics used.
In order to reduce the spread of these infections, healthcare facilities must follow the correct standards for infection prevention. There must be a system where all hospitals report rates of hospital-acquired infections to the State government. Ideally, the data should be made public. Currently, all NABH hospitals collect this data every month and take measures to reduce hospital-acquired infections. But it is crucial that all hospitals follow suit and share the data with the State. There will be greater and immediate long-term benefits of lowering AMR-related fatalities if measures to reduce hospital-acquired infections are successfully implemented.
Other essential measures, including rationalising antibiotic use in hospitals, banning the growth-promotional use of antibiotics in poultry farms, fish farms, and agriculture based on the already existing rules, are of paramount importance. Additionally, Kerala will do well if it supports and promotes the development of new antibiotics, diagnostics, and vaccines by entrepreneurs. Karnataka and Maharashtra-based startups have achieved remarkable progress in this domain. Startups based on novel service delivery models may help us make better use of our human resources when it comes to antibiotic stewardship and infection prevention.
While enforcing the OTC regulation is a welcome step, curbing antimicrobial resistance requires a multipronged approach, including reformations to physicians’ prescribing practices and mandating that hospitals report healthcare-associated infection rates. Strictly enforcing the OTC regulation without addressing the other issues, which are major drivers of antimicrobial resistance, may not help the cause. Enforcing the H1 rule is a relatively easy goal. The real challenge will be tackling the major drivers of AMR.
(Abdul Ghafur is coordinator, Chennai Declaration on AMR, and consultant in infectious diseases, Apollo Hospitals, Chennai)







