
Pressure has been mounting on the ACT government to commit to the establishment of a permanent gynaecological cancer surgery unit at Canberra Hospital, with more than 1700 people signing a petition in support of the clinic.
The Canberra Times revealed last month that time was running out to ensure women could access surgery for gynaecological cancers in the nation's capital.
But there are positive signs a clinic could be set up as Health Minister Rachel Stephen-Smith has said discussions to establish a centre were a priority.
A lack of a permanent service in the nation's capital has meant sufferers of gynaecological cancers have been forced to travel to Sydney to undergo gruelling surgery.
Doctors have been lobbying the territory government over the past three years for the permanent surgery unit but have struggled to receive a firm commitment.
The Royal Women's Hospital has provided a fortnightly surgery clinic to Canberra for the past 30 years but the sole visiting surgeon Dr Greg Robertson is set to retire at the end of this year.
Gynaecological oncology surgery is a rare sub-speciality and there are only about 60 people in Australia qualified in the field. Canberra local, Dr Leon Foster is prepared to set up in clinic in Canberra once his training in the incredibly rare speciality is completed this year.
Over recent weeks there have been discussions between Canberra Health Services and clinicians about the establishment of the service.
"This work is being prioritised and further updates will be provided as soon as possible," Ms Stephen-Smith said.
Several women who have experienced or had loved ones experience gynaecological cancers have spoken out in support of the service and have shared their experiences with The Canberra Times.
'It would have been much easier for me'
Wendy Dodd spoke to The Canberra Times last month after she had undergone surgery for her ovarian cancer. Since her surgery she has faced complications.
It has been an arduous process. Ms Dodd needed to have several phone calls with the Cancer Centre at the Royal Women Hospital in Sydney and has had lengthy waits at the emergency department.

"It would have been much easier for me if I had been able to speak to somebody who was on the surgical team and the support team directly rather than going through people in Canberra and then ringing somebody in Sydney and then they would give me advice," she said.
"The cancer centre here has a rapid assessment unit but they were understaffed at the time so they sent me back to two other people. The immediate post operative period was fairly difficult from that point of view."
Ms Dodd eventually secured an appointment with Dr Robertson and will need day surgery to fix her complications but she will need to wait for at least one month.
She said if she had been able to access a gynaecological oncologist sooner she may have received the correct diagnosis earlier.
'When mum was travelling back down the Hume it wasn't comfortable for her'
Jane Harriss' mother, Erica, died of ovarian cancer. Ms Harriss said the travel to Sydney for surgery had a significant physical, emotional and financial impact on sufferers of gynaecological cancers.
She said her mother was really unwell when she was diagnosed and travelling to Sydney added an extra burden.
For the first surgery, Erica had to stay in Sydney for 10 days and Ms Harriss took time off work to be with her.
"I was really busy at my job and it was really hard to actually take that time out from my perspective but of course I wouldn't have let Mum go through that all on her own," Ms Harriss said.
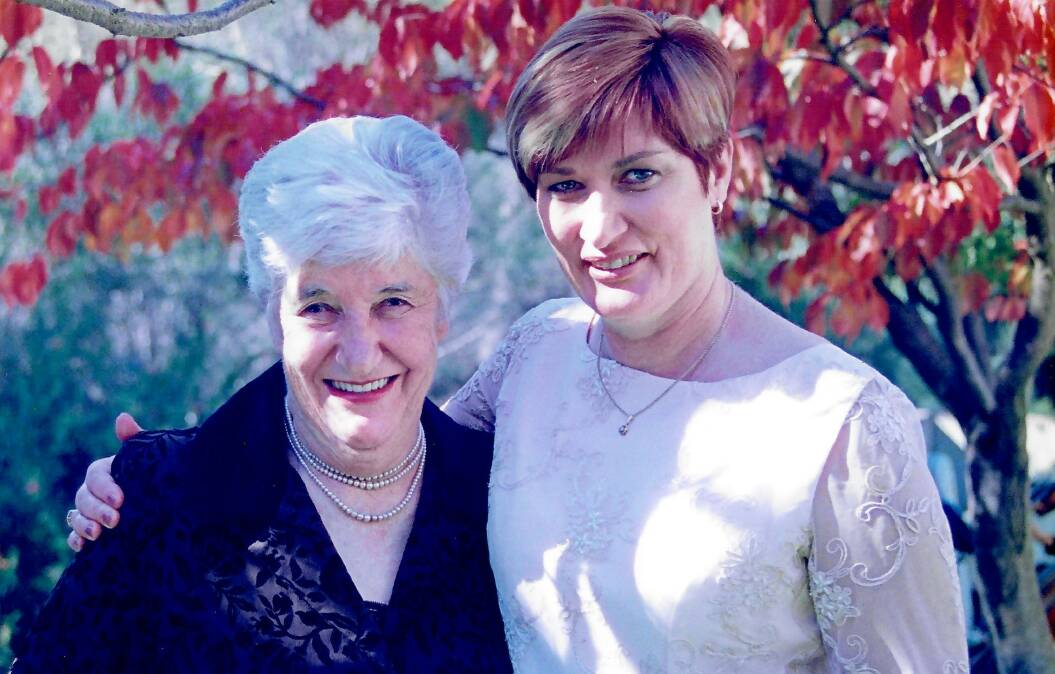
Unfortunately it was not the only time Erica had to travel to Sydney for gruelling surgery. She lived for seven years after being diagnosed and had several surgeries over that time.
"When mum was travelling back down the Hume it wasn't comfortable for her coming home back to Canberra after massive surgery," she said.
Ms Harriss also recalled how a Canberra ovarian cancer support group, which she ran, was approached about five years ago to help with fundraising for some surgical equipment Canberra Hospital would not fund. She said the group raised $22,000 to secure the equipment.
Ms Harriss said the issue had been raised over a long period.
"It has been raised for ages and there has always been this level of frustration about it, I know there's always demand on the health budget but this is pretty serious," she said.
"It's an important group within our community that need this service."
'I just can't fathom that'
Peggy Spratt was diagnosed with ovarian cancer following a visit to her general practitioner in 2019 to inquire about vaccines for an overseas holiday.
She made an offhand comment about having constipation, which triggered an alarm bell from her doctor who said it was a symptom of ovarian cancer. She was diagnosed shortly after.

Ms Spratt had a consultation with Dr Robertson who referred her to a team of surgeons in Newcastle where her son lived.
"Newcastle worked really well for me because I could be discharged to my son for surgical after care," she said.
"But how people can come back to Canberra in a car on the day they were discharged, I just can't fathom that."
'There is the population and demand for the service'
Cathy Rumble was the gynaecology oncology liaison nurse at the Canberra Hospital clinic for 20 years. She has been a strong advocate for the permanent centre.
Ms Rumble said the Canberra clinics were always fully booked and the doctors used to worry about the time constraints when seeing each new patient.
She wrote to Ms Stephen-Smith expressing her concerns.
"My concern is that if there is any delay in recruiting a new gynaecology oncologist the service will no longer exist and never be replaced once it is cut," Ms Rumble wrote in the letter.
"I am very aware that all hospitals in Australia are short of specialists including the ACT, it would be very difficult for ACT Health to try and recruit a gynaecology oncologist to Canberra especially once the service is cut.
"I am confident with my knowledge and experience of the current gynaecology oncology service at Canberra Hospital that there is the population and demand for the service now and into the future for ACT Health to fund our own Canberra-based gynaecology oncologist staff specialist."
We've made it a whole lot easier for you to have your say. Our new comment platform requires only one log-in to access articles and to join the discussion on The Canberra Times website. Find out how to register so you can enjoy civil, friendly and engaging discussions. See our moderation policy here.






