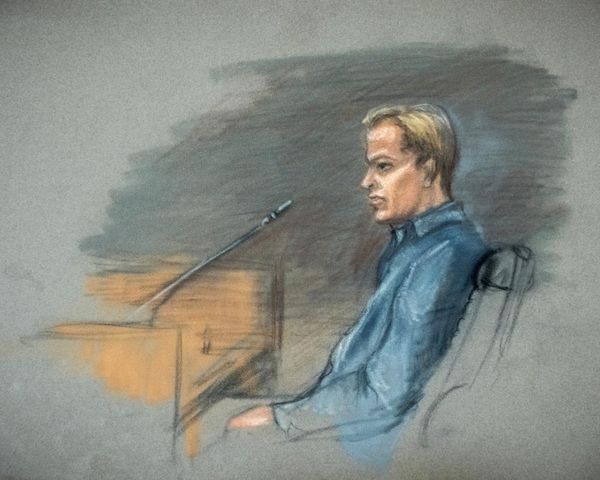
An infected wisdom tooth nearly killed Caitlin Alsop when it deteriorated into a "mystery" illness.
She was home alone and thought she'd bitten her tongue when her mouth worsened with swelling and pain.
"I was worried the lopsided tongue was a stroke," she says.
The then 23-year-old's health quickly deteriorated as she was left unable to speak or breathe.
"By the time we got to the hospital, my tongue was swollen, my mouth was jarred open and I had a blue-red rash all over my face," she says.
Doctors initially thought she was suffering an anaphylactic reaction so treated it with adrenaline but this only made her symptoms worse.
"I kept passing in and out of consciousness, I developed a fever and I couldn't breathe," Ms Alsop says. "I became a medical mystery."
She had to be intubated while her skin started to burn from the inside out "like a microwave". Her tongue blackened, nearing the point of amputation.
Her family was told to prepare for the worst.
Thanks to a doctor with a hunch, medical staff finally diagnosed severe sepsis as a result of an infected and impacted wisdom tooth.
"This infection I had known nothing about nearly took my life overnight," she says.
She was placed in a medically induced coma and given an antibiotic infusion until she recovered.
Five years later, Ms Alsop is using the terrifying experience to raise awareness of how common sepsis is.
"In nearly losing my tongue I have gained a voice and a cause of something I previously knew nothing about," she says.
At least 55,000 Australians develop sepsis each year and 8000 of them die from sepsis-related complications.
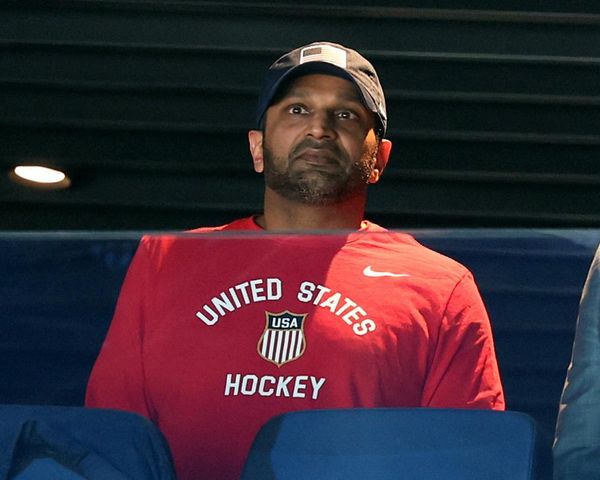
"People dying of sepsis is more common than people dying from road traffic accidents," University of Queensland researcher Professor Jason Roberts says.
After 30 years of research, a discovery showed a simple change in the way treatment is delivered could save thousands of lives and relieve the strain on the health system.
The University of Queensland and George Institute found a continuous intravenous infusion of antibiotics instead of short stints is more effective in curing infection.
The study found this could reduce the mortality rate at day 90 of a sepsis infection by two per cent, which researchers say is significant.
"Antibiotics usually kill bacteria in the first two-to-three days of therapy and after that, there isn't much more bacteria to kill," Prof Roberts says.
"So having a sustained effect out to three months is a really big deal."
The George Institute's Associate Professor Naomi Hammond says the change in protocols could save one life for every 26 patients treated.

The new method could be rolled out in hospitals across the world immediately.
"It will be life-saving for many people. These drugs are already available and it is just telling (hospitals) this is the best way to use them," she says.
Ms Alsop is celebrating the discovery.
"That simple change is something we can implement in so many hospitals, we can save lives and reach areas we haven't been able to reach previously," she says.
"You ask any person who had sepsis, who had a family go through it, or who lost someone, all we want is to prevent anyone else going through it."
Sepsis weighs a substantial burden on Australia's healthcare sector. Prof Roberts says many patients have to stay in care for long periods but the change in administration will ease the burden.
"This is something that it doesn't matter if you're in Brisbane, Sydney, Melbourne, Alice Springs or Charleville; it is an easily delivered intervention with existing resources," he says.
Ms Alsop hopes the breakthrough will also raise professional awareness so sepsis is front of mind when a patient arrives at hospital.
"Ask if it could be sepsis," she says.
The research has been published in The Journal of the American Medical Association.