When Traci Letts finally found the perfect shoes for her son Mike – a pair of white Nike trainers with a splash of green – the store didn’t have the right size. So she went to another.
“They had to be just right,” she said. “He always wanted to dress well.” The high-top shoes completed an outfit Letts had carefully selected: a grey tracksuit with a white T-shirt; they would be the final set of clothes he would wear. “I knew he’d want to be sent off that way.”
Mike, who she remembers as the “kindest and sweetest” of her three children, died on 3 February from a toxic overdose. He was 31 years old.
Canada’s westernmost province is trapped in an unprecedented public health crisis, which has torn apart families and left nearly 14,000 people dead from tainted, unregulated narcotics.
As grief and frustration mount, two activists are set to challenge the federal government in a British Columbia court, arguing that they should be allowed to supply pure drugs to users.
Their long-shot legal fight has highlighted the widening scope of a national catastrophe – and the increasingly desperate steps activists are taking to stop preventable deaths. When they appear in court on Thursday, Eris Nyx and Jeremy Kalicum will argue that Canada’s public health agency is ill-equipped to respond to the unfolding disaster – and that radical measures are necessary to stop people dying.
British Columbia’s opioid toxicity crisis first emerged around 2015, when synthetic forms of opioids and benzodiazepines began appearing in recreational drugs. The phenomenon mirrored a global trend in which psychoactive substances were used to bulk up shipments and increase the potency of heroin, cocaine and methamphetamines. After more than 500 deaths, the province declared a public health emergency the following year.
Last year was the worst on record: authorities in British Columbia recorded 2,539 suspected overdoses, the vast majority with fentanyl or fentanyl analogues in their body.
Engulfed by a crisis with no apparent end, community groups in Vancouver’s downtown east side – where the fatal overdose rate is nearly 30 times higher than the national average – have become increasingly desperate.
In 2022, the Drug User’s Liberation Front announced it would offer pure cocaine, methamphetamine and heroin to users as part of a “compassion club” to prevent overdose deaths.
“If you label people’s drugs such that they clearly indicate what a person is putting into their body, people won’t be overdosing,” Eris Nyx, a co-founder of the group, told the Guardian at the time. “No one takes more than they intend to take.”
The group applied for an exemption to Canada’s Controlled Drugs and Substances Act, so they could procure and sell drugs. With few options to legally purchase pharmaceutical-grade narcotics, the pair told Canada’s public health agency they would need to source the drugs through the dark web.
That admission led to a rejection of the request.
But despite the legal setback, the activists carried on selling pure drugs at cost price from their store in Vancouver’s downtown east side, in open defiance of the law. The experiment was cut short in October, after Vancouver police arrested – but didn’t charge – Nyx and Kalicum
On Thursday, the pair’s lawyers will challenge Health Canada’s decision not to approve the exemption, arguing the decision leaves people who use drugs “fully and directly exposed” to the toxicity crisis and violates two clauses of Canada’s charter of rights and freedoms: the right to life and a right to equal protection under the law.
“The deprivation of life and security of the person is stark,” the legal team wrote in its submission, which calls on the federal court to overturn the decision and to permit them to resume selling drugs.
The government acknowledges the mounting death toll from the crisis – and the need for new solutions. But for the government, illicit purchases through the dark web remain a step too far.
“Health Canada could not condone and support serious criminal activity, even in the context of the toxic drug crisis,” the government wrote in its legal submissions.
British Columbia has decriminalized – but not legalized – the possession of small amounts of illicit drugs. There are also safe injection sites in Vancouver, which give a space for users to consume drugs with the resources at hand to test drug purity and reverse overdose.
“People ask why, with decriminalization, the overdose rate keep going up. And the answer is very simple and straightforward. It’s because the drug supply has become increasingly toxic,” said Thomas Kerr, a professor in the department of medicine at the University of British Columbia. “We’re in what I would argue is the most catastrophic public health crisis we’ve experienced in Canada in the modern era.”
Nyx and Kalicum’s compassion club gave Kerr and his colleague Mary Clare Kennedy the chance to carry out what is thought to be the first-ever empirical, peer-reviewed study on the model.
After following 47 people over 14 months, the researchers found non-fatal overdoses dropped 49%. Non-fatal overdoses that required naloxone, suggesting the presence of fentanyl, dropped 63%.
“Our study shows that this model holds great promise,” said Kerr. “It’s really a time not to simply repeat what we’ve done in the past. ”
Letts – who volunteers with the advocacy group Moms Stop the Harm – worries thatmisinformation and moralizing about the nature of addiction are barriers that no court decision can overturn.
“People say. ‘Well, he chose to live that way.’ No, he didn’t choose to live that way,” she said. “You don’t just wake up one day and decide to start using an opioid. And even if you want to get treatment, there’s no magic wand you can wave. When people talk about treatment and recovery, what does that look like?”
For advocates and activists recovery and treatment – and preventing people from dying from toxic drugs – are two separate issues.
Last year the Conservative leader, Pierre Poilievre, prompted outrage on a visit to Vancouver, when he described the city as “hell on earth”, infuriating residents who accused him of using a vulnerable community as a political punching bag.
Such rhetoric strips people who use drugs of their humanity, said Letts, who pointed out that narcotics are consumed across society.
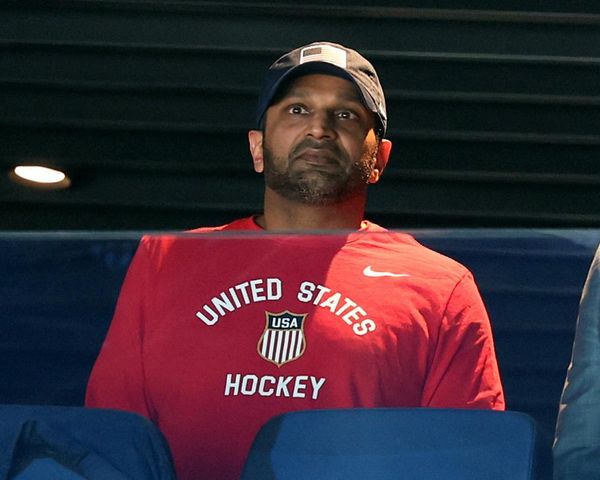
“The people dying are the children of lawyers and doctors. They’re hockey players or baseball players. They’re the parents that take their kids to hockey and baseball. They’re family men. They’re women trying to make it through the day, working two jobs.”
She remembers her son Mike as a hockey and baseball player, an animal lover and a quiet person who loved to cuddle.
“How do you describe what makes your child special? You can’t. It’s the moments together,” she said. “And I’ll miss those.”
A guaranteed safe supply of drugs could have saved Mike’s life, she said. While the mounting crisis has dampened her hopes of systemic change, she nonetheless remains hopeful the trajectory can change.
“In a way, stigma is the leading cause of death in this country,” said Letts. “And the biggest thing is most families don’t understand that this could easily happen to them.”