On two large screens in a small room in Northwick Park hospital, in north-west London director of operations John Ross is watching patients come and go in real-time.
Red and green lights flash as a patient is transferred into A&E from an ambulance; a dizzying column of names shift up and down as nurses are assigned to new patients.
It is a far cry from the noise and bustle of A&E, but this is the logistical nerve centre of the hospital.
From here, staff track the flow of patients through the hospital, find them a bed and ensure they don’t spread Covid.
“All of this goes unseen. People think that going to hospital is just about seeing a nurse or doctor and then going home - I wish it were that simple,” Mr Ross says.
“It is like a jigsaw puzzle. Everything has to be in the right order and people have to be getting the right care in the right wards.
“But that is just the easy part – then you find out that a lift has broken or a window has been smashed. We have no idea what is going to happen in a day.”
Winter at Northwick Park has been a serious challenge, with a shortage of beds and a relentless wave of daily admissions. The hospital, in Harrow, receives between 20-30 blue light ambulances per day – an ambulance arriving with a medical emergency - the highest figure in London.
A surge in flu, Covid-19 and Strep A, combined with staff absences, created the perfect storm over the New Year period, with some patients facing long waits for treatment in A&E.
At the core of the issue is a lack of beds, many of which are occupied by patients who are fit to be discharged but have no adequate social care package to be discharged into.
The fragmented bureaucracy of England’s social care system means staff often have to work through a mountain of forms just to get a medically fit patient out of hospital and into care.
“We have around 60 staff working behind the scenes on complex discharges just trying to get patients out of hospital,” Mr Ross says.
Gesturing at the screen, he adds: “All these people here are waiting for a bed. There’s no one in the corridor, which is good, but there are still too many people waiting in A&E.”

‘We won’t be able to cope without more beds’
While the hospital is currently able to cope with the daily influx of patients, bosses are anxious about the future. Without an urgent investment in a new critical care facility, they fear Northwick Park could struggle to cope next winter.
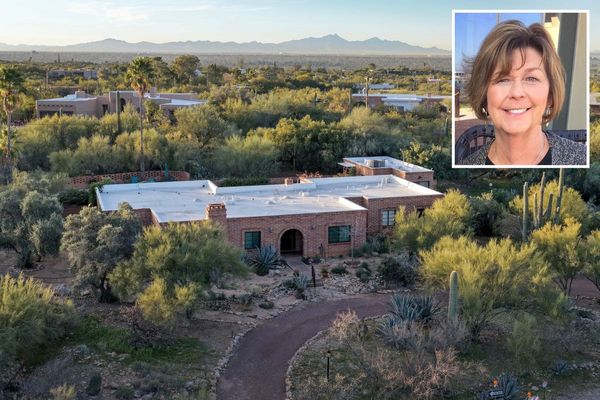
Pippa Nightingale, chief executive of London North West University Healthcare NHS Trust, is blunt about the scale of the problem and how to fix it.
“There are not enough beds for the number of patients coming to A&E. We can fix this in a simple way — by building a new ward — but the more sustainable option is to expand critical care. The borough of Brent had the highest mortality rate from Covid in London, so we are still running two wards as intensive care units.
“What we want to do is build a new state-of-the-art intensive care unit, which will release those two wards and make room for additional beds.”
Ms Nightingale is still chasing Whitehall for funding for the new facility following a visit by Health Secretary Steve Barclay in January.
But Northwick Park is not the only hospital in the capital in need of an injection of cash – last year the Standard revealed that £2.7 billion would be needed to fix the huge backlog of repairs across the capital.
She added: “We need capital funding for our buildings. Though we have an allocation, the estate is very old and it has the biggest backlog of maintenance of any London hospital.
“I simply have to do these works — we have to ensure the hospital is safe, has working lifts and meets fire regulations.”

‘Virtual wards help us manage patients at home’
To help free up beds, the hospital has been rolling out “virtual wards” for patients suffering from diabetes. These allow clinicians to monitor patients from home with the help of an app and a blood glucose meter.
Patients submit blood sugar readings multiple times a day and are able to contact nurses through the app or on the phone – meaning they do not need to stay in hospital if they are not severely ill.
“As long as a patient can take a blood sugar reading that is all they need,” explains Sharon McCarthy, a diabetes nurse consultant.
“The only criticism you get is patients who say ‘you just want the bed’ but usually once you actually talk through it with them they are really positive. They are getting more one to one intervention than if they actually stayed in the hospital as well as their own food and a good night’s sleep.”
Ministers see virtual wards as vital to solving the problem of delayed discharges in the long-term. NHS England plans to increase the capacity of virtual wards to 40-50 ‘beds’ per 100,000 population by the end of next year.
Northwick Park is currently using the scheme for diabetes and heart failure and is supporting other London hospitals – including Chelsea and Westminster and Hillingdon – to set up their own wards. In less than six weeks, the number of patients on virtual wards has quadrupled and bosses hope that they could soon be used for hundreds of patients.
Ms McCarthy hopes that, in time, the wards could be used to care for hundreds of patients and significantly ease pressure on the frontline.
“It’s a really clever initiative and saves so many beds. We don’t want diabetes to be keeping people in hospital.”

‘Early diagnosis is the holy grail of cancer treatment… but we need more staff’
Improving cancer treatment and reducing waiting times for diagnosis is a priority for Northwick Park – but recovering from the pandemic has been a challenge.
During the first and second wave, the number of two-week cancer referrals – the NHS standard for urgent cases - dropped by 60 per cent following a sharp fall in the number of GP appointments.
But at the same time, the number of people diagnosed with cancer saw an 8 per cent increase.
“It was a major incident without a debrief,” says Scott Rice, a consultant radiologist and the Divisional Medical Director at the hospital.
“Our workforce was exhausted by the first wave and then the second and third came. For us working in cancer, there was also the psychological trauma of seeing patients and thinking ‘I wish you had come in earlier’.”
The number of referrals is now up 5 per cent on pre-pandemic levels but the key for clinicians is catching cancer at an early stage, Dr Rice says. In order to meet the Government’s target of diagnosing 75 per cent of patients within 28 days, hospitals need more staff.
“The Government’s target of having more diagnostic equipment is needed and welcome but, as with the Nightingale hospitals, you need to have people to staff them.
“Radiographers are the unsung heroes of the NHS and there aren’t many of them being trained at undergraduate level. The person operating an MRI scanner is a very specialised member of staff. Even with international recruitment, we are struggling.”
I put it to Dr Rice that the Department of Health and Social Care (DHSC) claimed in a triumphant press release last month that there are more staff working in the NHS than ever before. It doesn’t appear to chime with those on the frontline who complain of barely-filled rotas and colleagues leaving every week.
“The question is about where we have got those people and what they are doing,” he responds. “If you are trying to backfill vacancies, you are effectively delivering staffing based on yesterday’s number today.
“Unless you look at your workforce, you can have all the scanners in the world but if there’s someone who is able to operate it that will be a limiting factor. As we detect more cancer, more patients are going to need to be followed up.”
For us working in cancer, there was also the psychological trauma of seeing patients and thinking ‘I wish you had come in earlier’
Like other NHS hospitals across the country, Northwick Park is bracing for a sustained period of pressure. Though the worst of the winter months may be over, they have already began to plan for the next.
But having faced the horrors of the pandemic, Mr Ross is confident that the hospital and its staff can cope with anything that gets thrown at them.
“It is tough. But the NHS always finds a way.”