Knowing whether a tumour might grow or spread to other parts of the body could be key to survival, research suggests.
Scientists say they are now one step closer to unlocking the ability to predict just that.
In a series of seven papers published in Nature and Nature Medicine, Cancer Research UK-funded researchers describe how changes to the DNA of cancer cells allow them to anticipate how the cells will behave in the future.
According to the research, this includes where and when the cancer will spread throughout the body.
TRACERx recognises that cancer is not static and the way we treat patients shouldn’t be either— Professor Charles Swanton, lead researcher
Scientists suggest the findings could one day allow doctors to use a blood test to predict how a patient’s cancer may grow and spread.
This would allow them to track the disease and rapidly adapt treatment in real time.
The studies also suggest it offers a possible route through which doctors could analyse the disease’s risk of returning following surgery.
Although lung cancer patients were the focus of the study, scientists say their findings could also be applied to other cancer types, such as skin cancer or kidney cancer.
These studies are the culmination of nine years of research from Cancer Research UK’s £14 million TRACERx study – the first long-term study of how lung cancer evolves.
The nationwide study involves more than 800 patients in clinical trials and a community of 250 investigators based at 13 hospital sites across the UK.
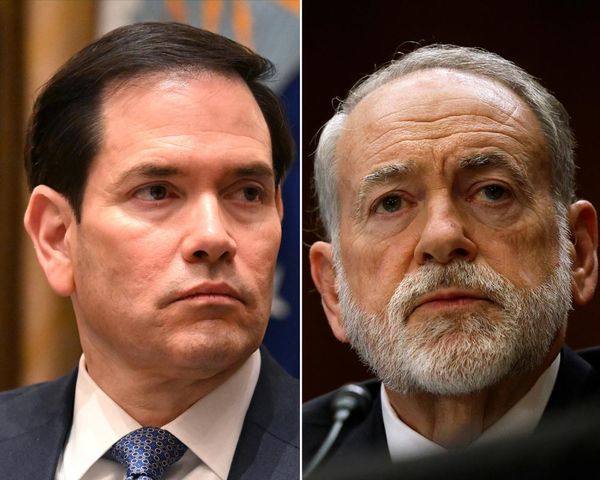
Lead researcher based at the Francis Crick Institute in London, UCL and Cancer Research UK’s chief clinician, Professor Charles Swanton, said: “TRACERx recognises that cancer is not static and the way we treat patients shouldn’t be either.
By looking at the tumour in its entirety, we can observe how these cell populations interact and even compete with one another, which is helping us to glean valuable insights into the likelihood that a tumour will return and when this might happen— Professor Charles Swanton, lead researcher
“What makes the TRACERx project particularly powerful is that it treats tumours as ever-changing ‘ecosystems’ made up of diverse cancer cell populations.
“By looking at the tumour in its entirety, we can observe how these cell populations interact and even compete with one another, which is helping us to glean valuable insights into the likelihood that a tumour will return and when this might happen.
“We can also observe how the tumour is likely to evolve over time, spread and respond to treatment, offering hope to millions of patients in the future.”
In the seven studies, researchers at the Crick and UCL followed 421 of the 842 TRACERx patients with non-small cell lung cancer (NSCLC) – the most common type of lung cancer – from when they were diagnosed to monitor how their tumours changed over time.
Across the papers the researchers made a number of findings, including that tumours can be made up of many different populations of cancer cells which carry sets of genes that are constantly changing.
The more diverse these tumours are, the more likely the patient’s cancer will return within one year of treatment.
They also found that some patterns of DNA changes in a patient’s tumour indicate what their cancer might do next.
These patterns could indicate to doctors which parts of a tumour might grow and spread to other parts of the body in the future.
A blood test that reads ctDNA could let doctors track someone’s cancer in real time, allowing them to personalise treatments to that patient— Dr Iain Foulkes, Cancer Research UK
Blood tests could be used to monitor these changes to tumour DNA in real time, helping doctors pick up on early signs that cancer is returning or not responding, researchers say.
The scientists also investigated whether they could track changes in the tumour and features of its genetic diversity without the need for surgery or biopsies.
By analysing DNA released into the bloodstream from tumour cells, known as circulating tumour DNA (ctDNA), they found that the presence of ctDNA in the blood before or after surgery suggested the patient’s cancer was highly likely to return in the future.
Further, the researchers also found that microscopic patterns created by the arrangement of tumour cells are linked with the risk of cancer returning.
Executive director of research at Cancer Research UK, Dr Iain Foulkes, said: “A blood test that reads ctDNA could let doctors track someone’s cancer in real time, allowing them to personalise treatments to that patient.
“Currently, the best option we have to monitor a patient’s tumour is to extract tissue either through a biopsy or during surgery. Both are invasive and time-consuming options which give us a limited snapshot of how that tumour is behaving at a given point in time.
“Analysis of ctDNA would give us a fuller picture of how the tumour is changing over the course of the patient’s disease using minimally invasive blood tests. It would allow doctors to treat people more proactively, taking swift action to change a treatment plan that’s not working.”