An estimated 295 million people suffer from visual impairment globally. Around 43 million of those people are living with blindness. While not every form of blindness can be cured, recent scientific breakthroughs have uncovered new ways to treat some forms of inherited blindness through gene therapy.
Jean Bennett is a gene therapy expert and a professor emeritus of ophthalmology at the University of Pennsylvania. She and her laboratory developed the first gene therapy drug for a genetic disease to be approved in the U.S. The drug, Luxturna, treats patients with biallelic RPE65 mutation-associated retinal dystrophy, a rare genetic disorder that causes visual impairments and blindness in patients early in life.
In March, Bennett spoke at the 2023 Imagine Solutions Conference in Naples, Florida, about what gene therapy is, why it matters, and the success she and her team have had helping the blind to see. The Conversation caught up with Bennett after the conference. Her edited answers are below.
What is gene therapy and how does it work?
Gene therapy is a set of techniques that harness DNA or RNA to treat or prevent disease. Gene therapy treats disease in three primary ways: by substituting a disease-causing gene with a healthy new or modified copy of that gene; turning genes on or off; and injecting a new or modified gene into the body.
How has gene therapy changed how doctors treat genetic eye diseases and blindness?
In the past, many doctors did not think it necessary to identify the genetic basis of eye disease because treatment was not yet available. However, a few specialists, including me and my collaborators, identified these defects in our research, convinced that someday treatment would be made possible. Over time, we were able to create a treatment designed for individuals with particular gene defects that lead to congenital blindness.
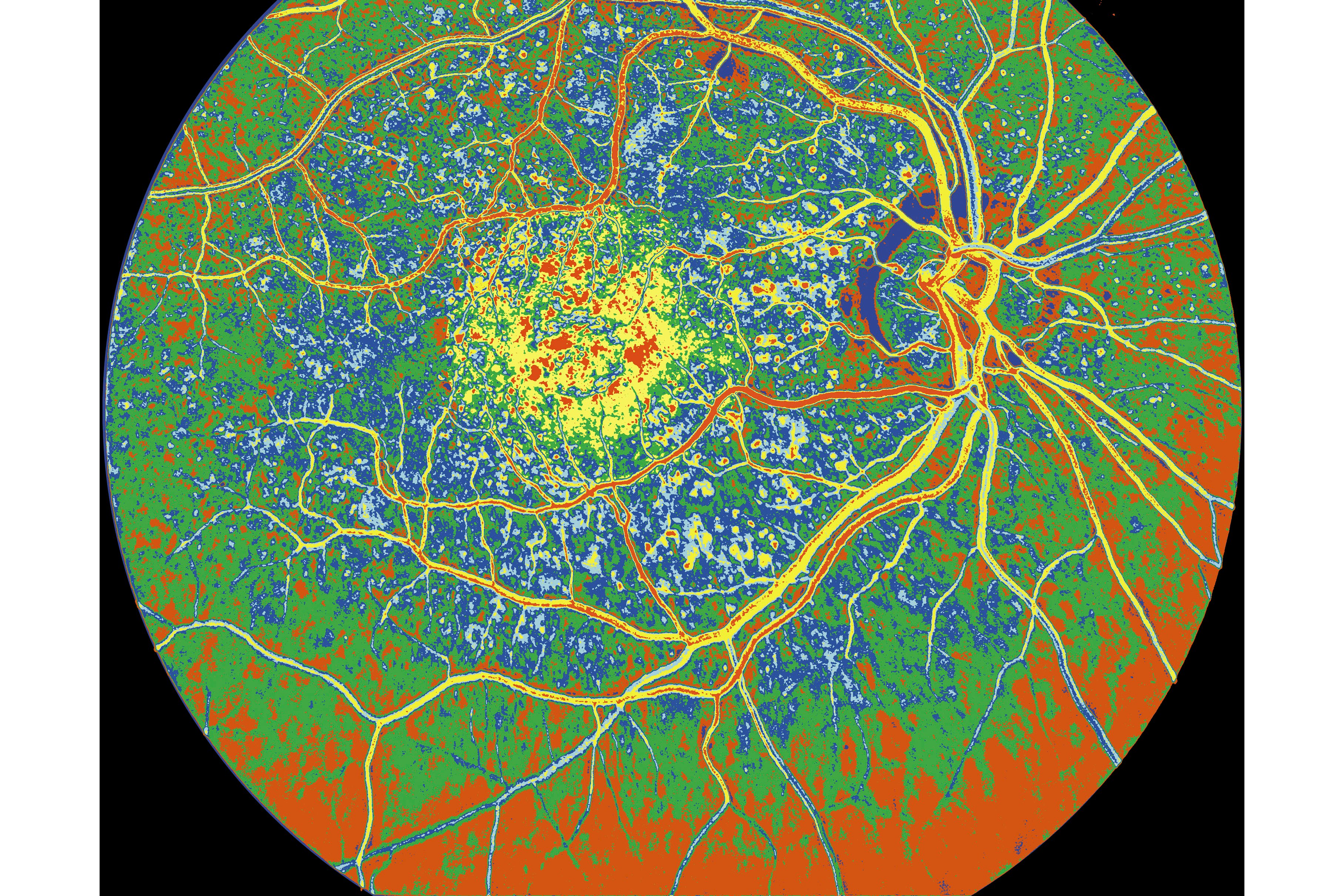
This development of gene therapy for inherited disease has inspired other groups around the world to initiate clinical trials targeting other genetic forms of blindness, such as choroideremia, achromatopsia, retinitis pigmentosa and even age-related macular degeneration, all of which lead to vision loss. There are at least 40 clinical trials enrolling patients with other genetic forms of blinding disease.
Gene therapy treatments are now available in pharmacies and operating rooms all over the world.
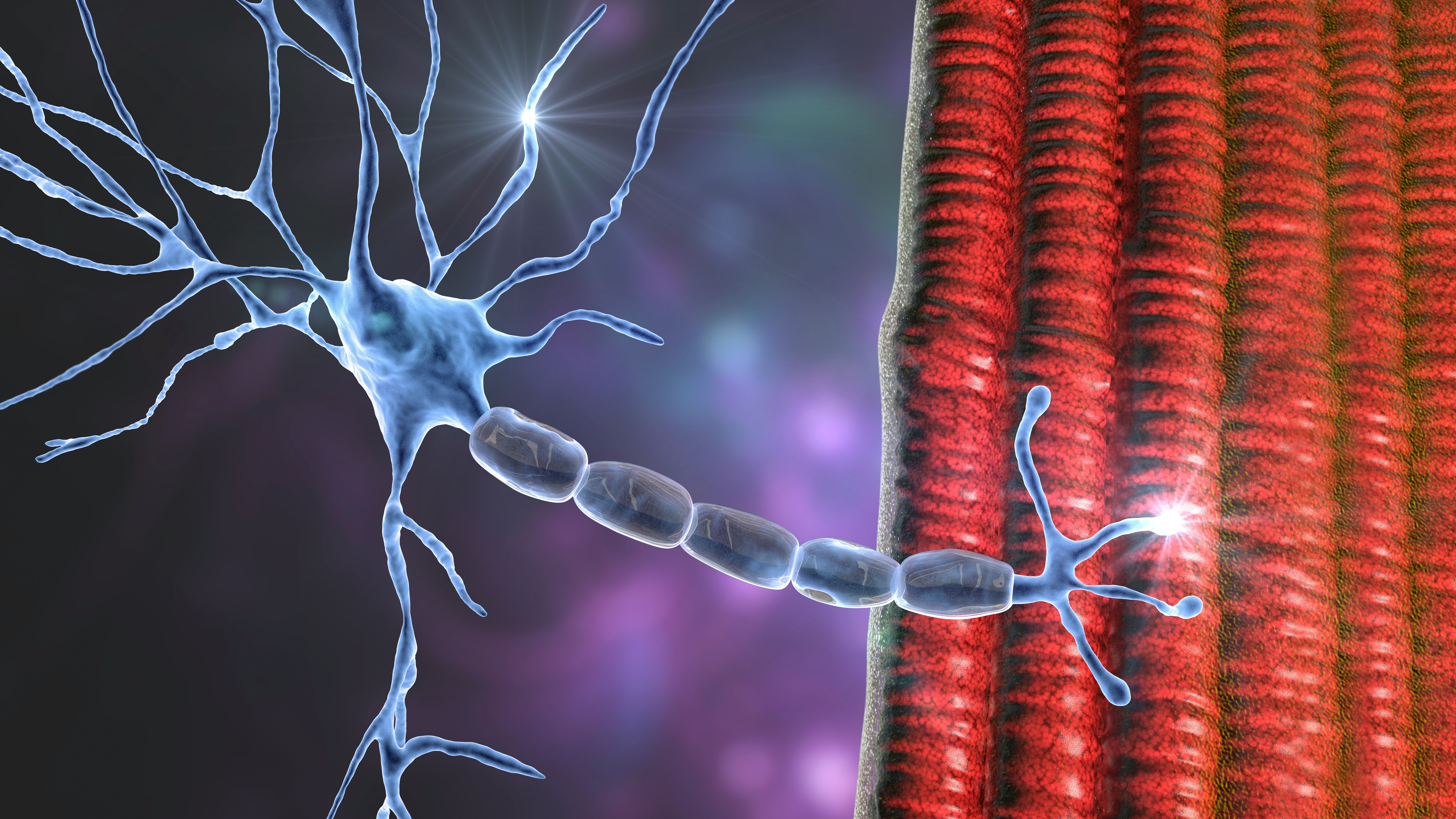
Gene therapy is even being used to restore vision to people whose photoreceptors — the cells in the retina that respond to light — have completely degenerated. This approach uses optogenetic therapy, which aims to revive those degenerated photoreceptors by adding light-sensing molecules to cells, thereby drastically improving a person’s vision.
You created one of the first gene therapies approved in the US. What is the current state of the clinical use of gene therapy?
There are now many approved gene therapies in the U.S., but the majority are combined with cell therapies in which a cell is modified in a dish and then injected back into the patient.
The majority of those therapies target different forms of cancer, although there are several for devastating inherited diseases. The drug Skysona is a new injectable gene therapy medication that treats boys ages 4 to 17 with cerebral adrenoleukodystrophy, a genetic disease in which a buildup of very long-chain fatty acids in the brain can lead to death.
The gene therapy that my team and I developed was the first FDA-approved project involving injection of a gene therapy directly into a person — in this case, into the retina. Only one other FDA-approved gene therapy is directly administered to the body — one that targets spinal muscular atrophy, a disease that causes progressive muscle weakness and eventually death. The drug, Zolgensma, is injected intravenously into babies and children diagnosed with the disease, allowing them to live as healthy, active children.
There are now more than two dozen FDA-approved cell and gene therapies, including CAR T-cell therapies — in which T cells, a type of immune system cells, are modified in the laboratory to better attack cancer cells in the body — and therapies for various blood diseases.
What are you currently working on that you’re most excited about?
I am very excited about some upcoming clinical trials that my team will soon initiate to target some other devastating blinding diseases. We will incorporate a new test of functional vision — how your eyes, brain and the visual pathways between them work together to help a person move in the world.
This test utilizes a virtual reality game that is not only fun for the user but promises to provide an objective measure of the person’s functional vision. I hope that our virtual reality test will inform us of any potential benefits from the treatments and also serve as a useful outcome measure for other gene and cell therapy clinical trials involving vision.

What are the biggest challenges gene therapy faces?
The biggest challenges involve systemic diseases, or diseases affecting the entire body rather than a single organ or body part. For those diseases, super-high doses of gene therapy reagents must be delivered. Such diseases involve not only technical challenges — such as how to manufacture enormous amounts of gene therapy compounds without contaminating them — but also difficulties ensuring that the treatment targets diseased tissues without causing toxic immune side effects. That level of a problem does not exist with the eye, where relatively small doses are used and exposure to the rest of the body is limited.
Another challenge is how to address diseases in which the target gene is very large. Current approaches to delivering treatments into cells lack the capacity to hold large genes.
Cost remains a key issue in this effort — gene therapy drugs are enormously expensive. As drug manufacturers are able to refine this technique, gene therapy drugs may become more commonplace, causing their price to drop as a result.
This article was originally published on The Conversation by Jean Bennett at the University of Pennsylvania. Read the original article here.







