Dr. Josie Tenore and Paul Hinds were introduced by a mutual friend in 2017 and hadn’t been going out long when she laid down the law: He had to get a physical.
“I don’t date people who don’t take care of their health,” said Tenore, who practices cosmetic dermatology and functional medicine in Highland Park.
One of Hinds’ blood tests that summer came back with an alarming result: His prostate-specific antigen, or PSA, level was very high. A biopsy confirmed he had advanced prostate cancer.
There aren’t a lot of comfortable alternatives for treating prostate cancer, which generally progresses as long as testosterone levels remain high. Marijuana appears to lower testosterone levels. So, after his diagnosis, Hinds dosed a liquid form of cannabis for several weeks. That cut his PSA in half, but Hinds, a cybersecurity expert who likes yoga and bicycling, “was stoned out of his mind and couldn’t function,” according to Tenore.
With Tenore guiding his decisions, Hinds next tried a procedure called high-frequency ultrasound treatment, but it failed. In the summer of 2019, doctors at the University of Chicago Medical Center removed his prostate gland.
Still, the PSA levels climbed again, and doctors assessed that the cancer had metastasized. The only alternative was to drastically lower Hinds’ testosterone levels — either via surgery or drugs that block all testosterone. In May 2021, Hinds got his first intramuscular shot of Lupron Depot, a brand name for leuprolide, designed to suppress the prostate gland’s release of the hormone for three months. That August, he got his second shot.
And then the bills came. Here’s a look at how things proceeded.
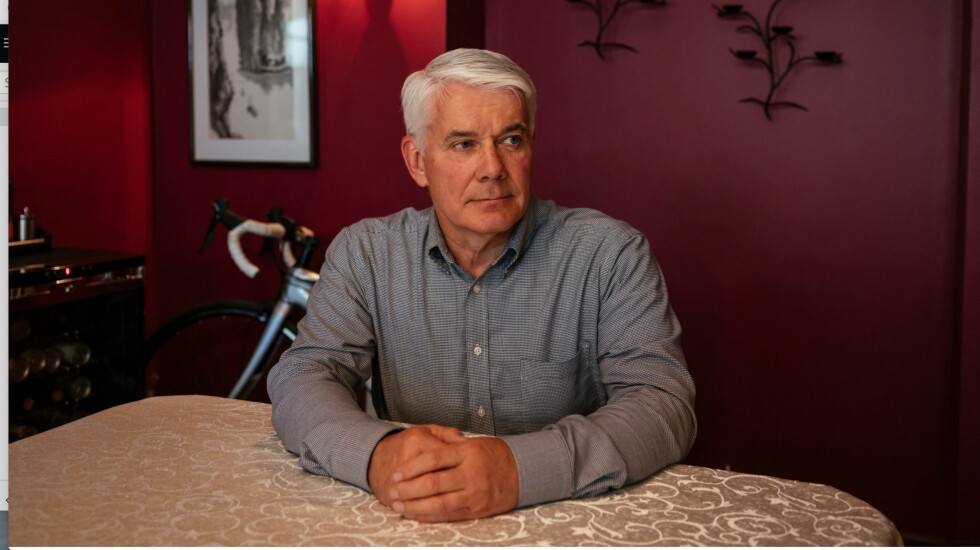
The patient: Paul Hinds, now 60, who lives in Highland Park, is covered by United Healthcare through a COBRA plan from his former employer.
Medical service: Two three-month Lupron Depot injections for metastatic prostate cancer.
Service provider: University of Chicago Medicine, a 900-physician nonprofit system that includes the 811-bed University of Chicago Medical Center, Ingalls Memorial Hospital in Harvey, the Pritzker School of Medicine and outpatient clinics and physician offices throughout the Chicago area.
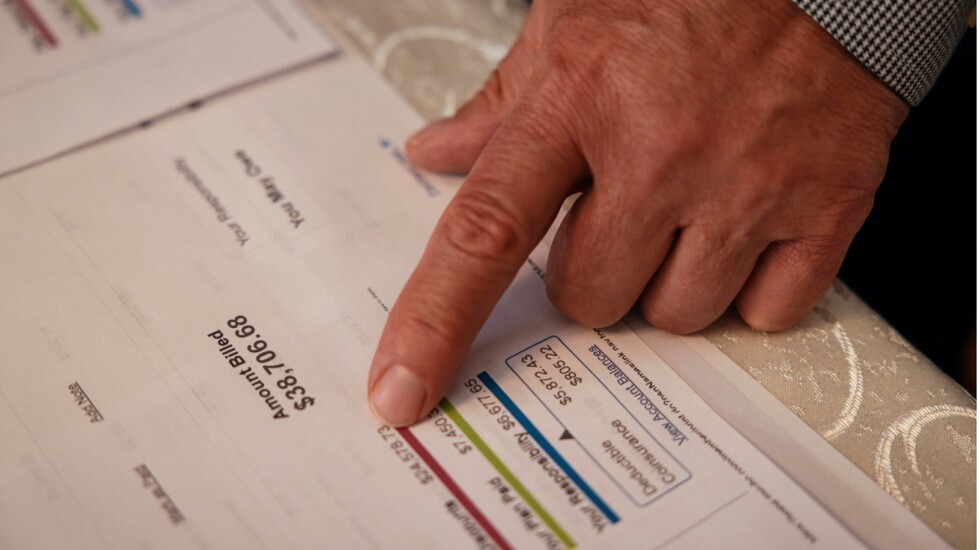
Total bill: $73,812 for the two shots — $35,414 for the first, $38,398 for the second —, including lab work and physician charges. United Healthcare’s negotiated rate for the two shots and associated fees was $27,568, of which the insurer paid $19,567. After Hinds haggled with the hospital and insurer for more than a year, his share of the bills was determined to be nearly $7,000.
What gives: The first issue is unrelenting price increases on old drugs that have remained branded as manufacturers find ways to extend patents for decades and maintain sales through marketing.
Though Lupron was invented in 1973, its manufacturer got patent extensions in 1989 by offering a slow-release version. Drugmakers commonly use this tactic to extend their exclusive rights to sell a product.
The development of Lupron Depot as an intramuscular shot that suppressed testosterone for months at a time improved patient compliance and also enabled its maker, Abbott Laboratories, and its Japanese partner, Takeda, to extend their patents on the drug into the 2000s, said Dr. Gerald Weisberg, a former Abbott scientist who has been critical of the North Chicago-based company’s pricing policies.
In subsequent years, Abbott and Takeda, in a joint venture called TAP Pharmaceuticals, steadily marked up the price of their slow-release product. In 2000, the average wholesale U.S. price for a three-month shot was $1,245; the current figure is $5,866. (It is now manufactured in the United States by North Chicago-based AbbVie.)
In the United Kingdom, where health care is generally free and Takeda sells the drug under the name Prostap, all physicians can buy a three-month dose for about $260.
It’s likely that University of Chicago Medicine, where Hinds got his shots, paid something close to the British price. That’s because the hospital on the South Side participates in a federal program called 340B, which allows hospitals that serve low-income populations to purchase drugs at deep discounts.
Lupron Depot is given as a simple injection into the muscle. It takes minutes for a nurse or doctor to administer. Yet hospital systems like University of Chicago Medicine can and typically do charge lavishly for such services to enhance their revenues, said Morgan Henderson, principal data scientist for the Hilltop Institute at the University of Maryland-Baltimore County.
University of Chicago Medicine declined to say what it paid for the drug.
While U.S. drugmakers can price their drugs however they please, TAP has gotten into trouble for its Lupron sales policies in the past. In 2001, after a Justice Department probe, it paid an $875 million settlement for illegally stimulating sales by giving urologists free and discounted vials of the drug while enabling them to charge Medicare full price.
Since then, many other drugs aimed at lowering testosterone levels have entered the market, including a pill, relugolix — brand name Orgovyx. So why wouldn’t a patient use them?
Lupron Depot is long-acting, is easy to prepare and store and employs a small needle, which some patients prefer, said Dr. Brian McNeil, chief of urology at University Hospital of Brooklyn. Orgovyx is convenient, but “a patient has to be very compliant,” McNeill said. “They have to take it every day around the same time. Some people just forget.”
But there is another important factor that might well explain Lupron Depot’s ongoing popularity among medical providers: Doctors and hospitals can make tens of thousands of dollars for each visit by marking up its price and administration fees — as they did with Hinds. If they merely write a prescription for a drug that can be taken at home, they make nothing.
Asked about this high patient charge and the possibility of using alternatives, United Healthcare spokesperson Maria Gordon Shydlo said payment was “appropriately based on the hospital’s contract and the member’s benefit plan” and that the insurer encourages customers to shop around for the best quality and price.
Resolution: In addition to leaving Hinds listless, the Lupron Depot shots were — literally — a pain in the rear end.
“Each time, he was miserable for two weeks,” Tenore said.
After looking over his first bill for the Lupron shot, Tenore told Hinds he should ask his doctor whether there was a less expensive drug that was easier to take.
After the second shot, in August 2021, a pharmacist told him he could instead receive the pill. His doctor prescribed Hinds three months’ worth of Orgovyx last November, for which he paid $216, and the insurer paid over $6,000.
The drug’s list price is about $2,700 a month.
There is evidence that Orgovyx works a little better than leuprolide.
Orgovyx was a “no-brainer,” Hinds said. “Why would you want a sore ass for two weeks when you can take a pill that kicks in sooner, functions the same way and clears your body of testosterone faster?”
While Orgovyx increasingly is used for prostate cancer, Lupron and other injections usually remain the standard of care, hospital spokesperson Ashley Heher said. Clinicians “work with patients to determine what treatments are the most medically effective and, when necessary, to find reasonable alternatives that may be less financially burdensome due to insurance coverage limitations.”
Hinds was baffled by the charges. During months of calls and emails, the hospital reversed and then reapplied part of the charge and then in July agreed to a $666.34 monthly payment plan.
After Hinds had made two payments, though, the hospital said Aug. 29 it was canceling the agreement and sending the remainder of his bill to a collection agency.
Two weeks later, the hospital reinstated the payment plan — after KHN asked about the cancellation.
Hinds remains active, though he said he has shortened his bike rides from 50 or 60 miles to about 30 miles.
He’s grateful to have Tenore as a free consultant and empathizes with those who lack a knowledgeable guide through their disease and health care’s financial maze.
“I’ve got Dr. Josie as an advocate who knows the system,” he said.
Paul Hinds, a cybersecurity expert who likes yoga and bicycling, was diagnosed with prostate cancer about five years ago. He tried multiple treatments before turning to intramuscular shots of Lupron Depot to suppress testosterone. Two shots, lasting three months each, came with a price tag of $73,812, including lab work and physician charges. (Taylor Glascock for KHN)
The takeaway: If you are prescribed an infusion or injection, ask your physician whether there are cheaper oral medications to treat your condition. Also, many drugs that are given by injection — ones that are given subcutaneously rather than into a muscle — can be administered by a patient at home, avoiding hefty administration fees. Drugs like Dupixent for eczema fall into this category.
Keep in mind that where you get treatment could make a big difference in the charges: A study found that leading U.S. cancer centers charge enormous markups to private insurers for drug injections or infusions. Another study found that hospital systems charge an average of 86% more than private clinics for cancer drug infusions. And the percentage of cancer infusions done in hospital-operated clinics increased from 6% in 2004 to 43% in 2014 and has risen since.
Under a law that took effect in 2021, hospitals are required to list their charges, though they currently do so in a way that is not user-friendly. But it’s worth taking a look at the price list — the hospital “chargemaster” — to try to decipher the pricing and markup for your medicine. If you’re about to get an injection, infusion or procedure done in a hospital system, ask ahead of time for an estimate of what you will owe.







