There are over 7,000 rare diseases that collectively affect more than 30 million Americans. Children and families struggling with these diseases need treatments — and hope. We're urging the U.S. Food and Drug Administration to use regulatory tools, such as its accelerated approval pathway, to speed up the development and approval of treatments.
But to date, FDA regulators haven't done so, even for promising drug candidates.
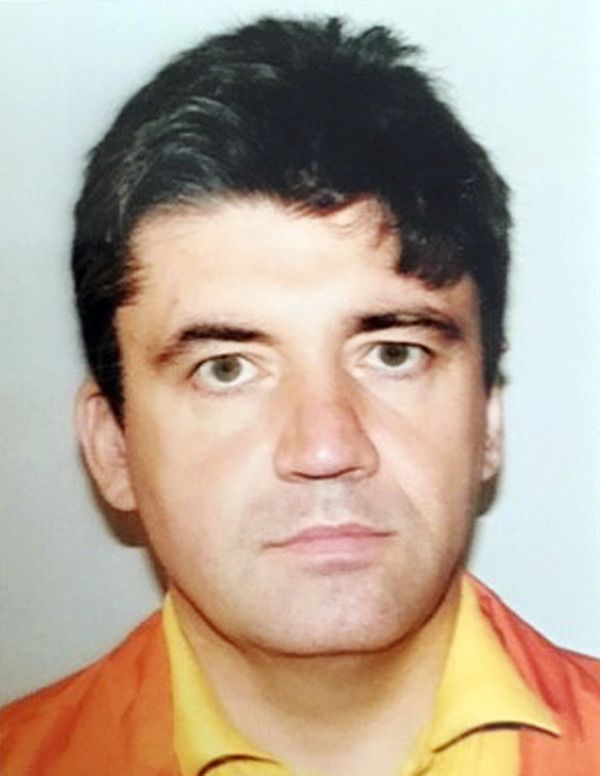
We are regrettably well-acquainted with one of these disease groups: a class of genetic metabolic conditions called the mucopolysaccharidoses, or MPSs. One of us — Mark Dant — has a child born with an MPS disorder. Dr. Matthew Ellinwood, a translational researcher and the chief scientific officer at the National MPS Society, has spent his career researching MPS.
The MPSs typically arise in infancy and early childhood. The 12 MPS subtypes cumulatively affect one in every 25,000 children. They cause developmental delay, chronic pain, enlarged organs and early death in severe cases.
Sadly, countless other rare disease patients are in a similar predicament. Regulators rarely approve promising treatments without time-consuming, logistically impossible and ethically-flawed clinical trials, even in cases when alternative regulatory pathways may exist.
This must change. Drug regulators must expand the use of accelerated approval for rare disease treatments. Lives hang in the balance.
For diseases like MPS, few approved treatments exist. That's not necessarily because scientists and clinicians don't know how to treat them. It's because the traditional FDA approval process wasn't built for rare diseases.
To get a green light from the FDA using the traditional approval process, new drugs must undergo two randomized, placebo-controlled clinical trials that confirm safety and clinical benefit — usually defined as a reduction in symptoms. Trials often include thousands of participants.
In the United States, rare diseases are defined as those affecting fewer than 200,000 Americans. For individual MPS syndromes, patients likely number in the hundreds.
That essentially makes finding enough patients to enroll in traditional trials impossible. Often, researchers are forced to recruit participants internationally, adding additional expenses and obstacles.
Moreover, disorders like the MPSs progress quickly from the time a child is born. Patients available to enroll in trials may already display severe symptoms, making traditional trials particularly challenging.
This situation is especially evident with MPS III — a fatal neurodegenerative disease also known as Sanfilippo syndrome. Children with MPS III experience symptoms resembling both autism and Alzheimer's disease. They typically live just 10 to 20 years.
For patients with Sanfilippo syndrome, effective treatments might not show a measurable clinical benefit within the two-year span of a traditional clinical trial. As a result, therapies that show enormous potential are abandoned.
The FDA has a separate approval pathway, the accelerated approval process, for diseases that aren't suited to standard clinical trials. Drugs applying for this kind of approval don't need to show a measurable clinical benefit, such as a reduction in symptoms. Instead, drugs can be approved based on a "surrogate endpoint," also known as a "biomarker."
In these cases, medical tests may show an outcome associated with improvement in patients. That might allow for a drug to receive FDA approval, which has long been a serious challenge for medicines treating complex, rare diseases like MPS.
Since its implementation in 1992, accelerated approval has been hugely effective. It was used to greenlight AZT, the first effective antiretroviral for HIV and AIDS.
A widely-accepted biomarker exists for Sanfilippo syndrome and related MPSs. Studies show that a reduction in heparan sulfate, a complex type of carbohydrate found in the body's tissues, is likely to produce positive clinical outcomes in patients.
The existence of this biomarker makes drugs for Sanfilippo syndrome ideal candidates for accelerated approval. Such an approval could be based on evidence that a drug lowers a patient's heparan sulfate levels. In fact, the FDA itself has already issued a guidance acknowledging heparan sulfate's potential as a biomarker.
Our collective understanding of MPS has progressed significantly over recent decades, and numerous treatments are now in development. But to the dismay of patients and families, none of these drug candidates have been granted accelerated approval.
Developing new rare-disease treatments is daunting. Given the small pool of potential patients, rare disease drug developers have a slim chance of recouping their R&D investment. The fact that MPS treatments haven't received accelerated approval has thrown some programs into serious doubt — and caused others to shut down altogether.
The science behind heparan sulfate and MPSs is clear. It's imperative that the FDA review promising drugs appropriately via accelerated approval. Doing so will not only save patients, but also reignite interest in rare-disease research more broadly.
Will the FDA act? More than 30 million Americans with rare diseases are watching.