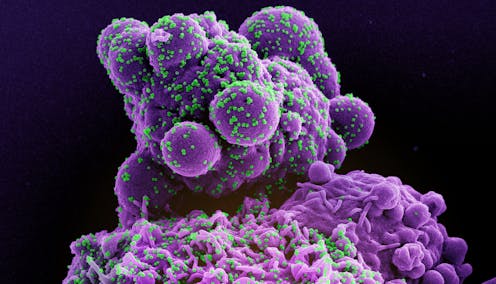
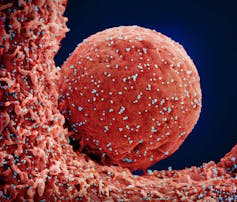
It’s been almost four years since the first human cases of COVID-19 infection caused by SARS-CoV-2 were reported.
Though the global health emergency was declared over on May 5, 2023, COVID-19 remains a major public health threat. As we enter the fall/winter respiratory virus season, it’s a good time to review current COVID-19 risks and recommendations.
What are the current COVID subvariants in circulation?
The dynamically evolving nature of SARS-CoV-2 represents a major hurdle for vaccine scientists. Omicron XBB.1.5 was the globally dominant subvariant during the first half of 2023, one which led to the development of the updated mRNA vaccines.
However, the predominant subvariants circulating in the United States, United Kingdom, European Union and Canada at the time of writing include Omicron subvariants EG.5, FL1.5.1, XBB.1.16, XBB.1.9 and XBB.2.3.
Do they cause serious illness?
The capability of currently circulating subvariants of SARS-CoV-2 to cause serious illness appears similar to that of other Omicron lineages, including XBB.1.5. The main risk factors for developing more than just a mild respiratory tract infection include increasing age, immunosuppression, cancer, pregnancy and the presence of chronic medical conditions.
Comorbidities such as diabetes, obesity and diseases of the lungs, heart, liver, kidneys and neurologic system are all risk factors for hospitalization, critical illness and death due to COVID-19.
In adults, the odds of dying with COVID-19 increase by approximately three- to six-fold with obesity and four-fold with pulmonary disease. In children, the odds of dying increases by about 63-fold with obesity, 20-fold with Down’s syndrome and 1.4-fold with asthma. In adults with COVID-19 infection, men are almost twice as likely to die as women.
Long COVID (also known as post COVID-19 condition) is one of the most discussed complications of SARS-CoV-2 infection. However, it is rare in children and adolescents without chronic health conditions. Furthermore, vaccination does not appear to prevent long-COVID in children.
Is there a possibility of a fall surge in COVID-19 cases?
In contrast to pandemics, which are global in nature and involve sustained virus transmission, outbreaks are time-limited and geographically restricted.
During the last three respiratory virus seasons in the U.S. and Europe, COVID-19 transmission patterns were somewhat reminiscent of seasonal influenza. The fall/winter outbreaks of COVID-19 were characterized by a sudden increase in infection rates above the baseline pandemic level.
These observations, along with recent wastewater surveillance and clinical data, suggest that a spike in hospitalizations and deaths from COVID-19 is likely to occur this fall and winter.
Are current vaccines protective?
In September 2023, policymakers in the U.S., the U.K., Canada and the EU announced the approval of updated COVID-19 mRNA vaccines.
These “next generation” products were formulated to target the XBB.1.5 subvariant. Unpublished pre-clinical studies that led to regulatory approval have demonstrated these vaccines to be safe and efficacious in all age groups.
The astonishing ability of the virus to mutate at every given opportunity has made it extremely challenging for scientists to develop a vaccine that offers long-term protection. The XBB.1.5 subvariant now accounts for only two to five per cent of circulating SARS-CoV-2 viruses, and is on the verge of becoming extinct. Newer circulating subvariants such as EG.5 possess novel mutations that may reduce the effectiveness of vaccine-mediated immunity.
What are the current vaccine recommendations?
Recommendations for the updated vaccines vary according to country/region, vaccine product, presence of chronic health problems, age and history of prior COVID-19 vaccination or infection.
Public health authorities in Canada, the U.K. and the EU have strongly emphasized the need to prioritize vaccination for those at highest risk of illness, including those providing essential community services.
In contrast, the U.S. Food & Drug Administration has provided the general public with vaccine recommendations that are not risk-stratified.
Dosing guidelines for these newer vaccines are summarized in the table below:
How can I protect my health?
In addition to vaccination, standard infection control practices are recommended at all times to prevent the acquisition and transmission of respiratory tract viruses such as SARS-CoV-2. These measures include staying at home when ill, wearing a surgical or N95 mask in crowded indoor areas and frequent hand-washing.
Research evidence supports a non-universal vaccination strategy that focuses on high-risk individuals. Healthy children and adolescents are low-priority candidates for COVID-19 vaccination according to the World Health Organization and renowned experts.
The mortality rate for unvaccinated children under the age of 18 years is around 1/400,000, with most deaths occurring in those with comorbidities. Therefore, parents and their children should consult with their health-care provider for personalized recommendations.
Public health messaging for vaccine-preventable illnesses often ignores other health-promoting activities such as regular physical exercise, a healthy diet, restful sleep and avoidance of harmful substances (smoking, alcohol, illicit drugs). These lifestyle practices can improve and protect health, but are not a substitute for vaccination.
What if I’m hesitant about getting a vaccine?
Research has clearly shown who is at greatest risk of developing severe COVID-19 illness, and who stands to benefit most from vaccination. Yet, misinformation may compel some high-risk individuals to avoid vaccination altogether.
Read more: How pharma can build trust in COVID-19 vaccines: Transparency on trials and side-effects
These doubts may be fuelled by a perceived lack of transparency of governments and the pharmaceutical industry. In these instances, a shared decision-making approach involving patients and their trusted health-care providers is recommended to dispel any myths about vaccines.
Sameer Elsayed does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.