For years, Martin Jugenburg—a Toronto-based plastic and reconstructive surgeon who goes by Dr. 6ix on social media—shared dozens of before-and-after photos and videos on Instagram of the altered bodies that had passed through his hands. There were tummy tucks, Brazilian butt lifts, and breast augmentations, all of them sorted into a kind of virtual assembly line for his thousands of followers to see.
But many of the women he featured in his posts—sometimes depicted post-op and sedated, their genitals and breasts blurred out—hadn’t consented to having their images circulated, according to an ongoing class action lawsuit, and some were only alerted of their presence online due to an investigation by CBC journalists. Unbeknownst to his patients and followers, investigators later found that Jugenburg was using a covert network of cameras in his clinic to perform a rigorous feat of surveillance, documenting thousands surgical procedures. Women who realized he had posted images of them told investigators they felt violated; they were upset, embarrassed, and distressed.
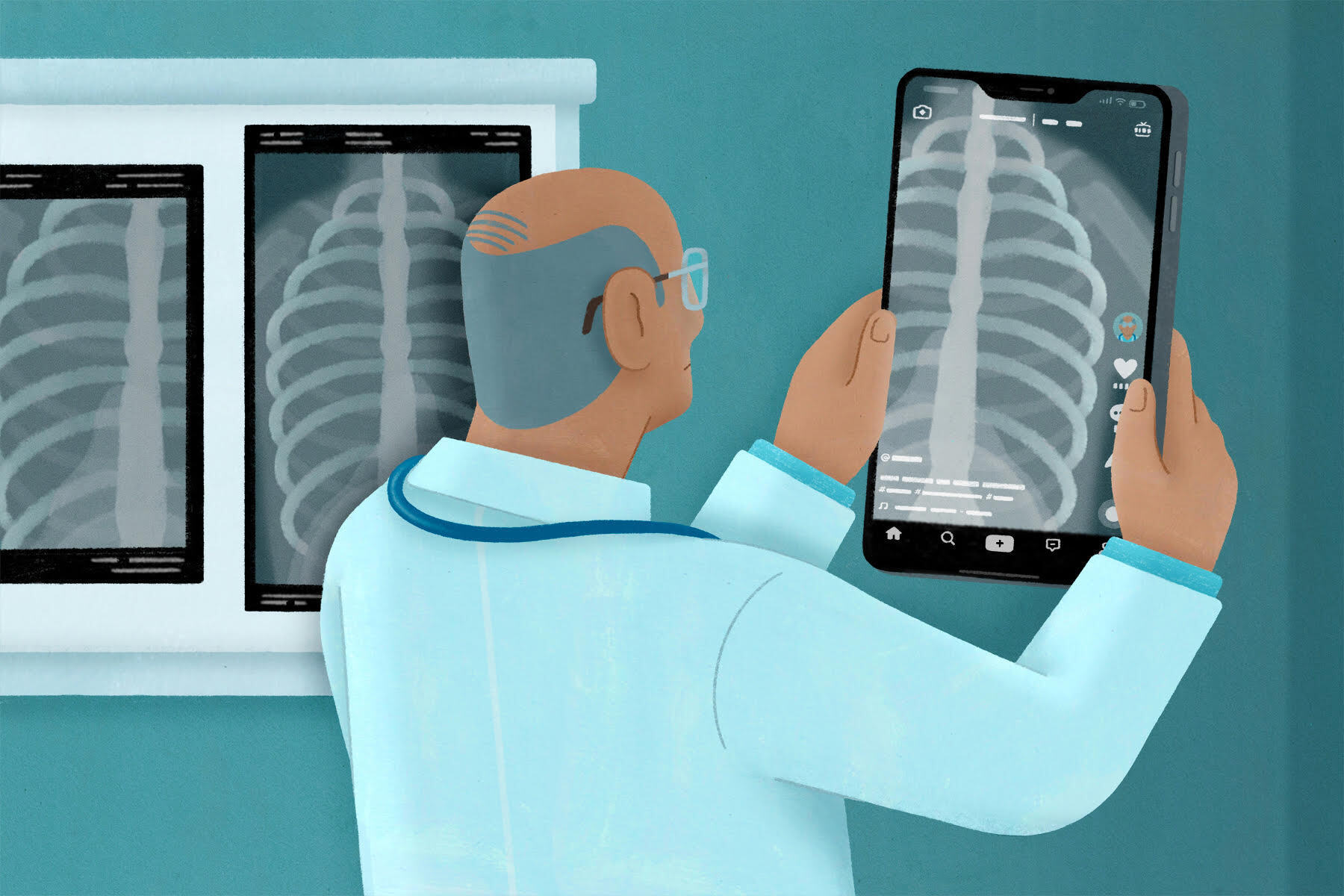
Dr. 6ix’s loose approach to respecting patient privacy on social media is hardly unusual in the world of “med Twitter” and “MedTok,” or medical TikTok. On Twitter, orthopedic surgeons complain about chronic pain “crazies,” nurses mock women who choose to give birth without an epidural, and doctors complain about “liars,” “Googlers,” and patients with conditions they are struggling to diagnose. TikTok is worse. In a post by someone with the username Nurse Johnn, whose derogatory skits about dementia patients he claims are fiction, the nurse mockingly dances in blue-green scrubs on a hospital bed, imitating someone under his care. One nurse filmed themselves holding the hand of a patient they said was dying of COVID-19. There is a video of someone in what appears to be a psychiatric crisis and another of a patient having their toenails cut. A Miami-based doctor posted about how he “walks in the footsteps of giants” in reference to porn star Johnny Sins, who impersonates a doctor having sex with his patients.
To scroll through many medical social media accounts is to wade into a virtual subculture where patients have become fodder for derision, their privacy and dignity regularly violated. But since there isn’t really any oversight of this virtual world, patients must bear the repercussions. Medical professionals spilling these traumatic, “hilarious” stories about their patients can lead to people not going to the doctor, says Shayna Hermann, a graduate student at the University of North Texas who studies criminology. This means the underlying health issue can “get worse and worse,” she adds—often with dire consequences.
The concealment of a patient’s medical information is an ancient custom, for such knowledge is a “holy secret,” according to the Hippocratic Oath. Medical students still refer to a doctrine of “doing no harm” that is based on the Hippocratic oath, and harm, to Hippocrates, included the dissemination of information shared between a patient and their doctor. Otherwise, trust in medicine could be undermined, disrupting treatment and diagnosis. Medicine is about acting but also about not acting.
The Enlightenment enshrined patient confidentiality as one of the formative values of the modern biomedical model. Ideals cherished under liberalism, like the individual’s right to autonomy over their body, would be impossible to respect without the guarantee that their medical records remained private. Those ideas would persist throughout the twentieth century. In 1948, the World Medical Association, an international body that now represents 115 medical associations worldwide, produced the Declaration of Geneva for the purposes of unifying an international standard for medical practice. The document reads: “I will respect the secrets that are confided in me, even after the patient has died.” Today, a patient’s right to privacy has been legally protected in both Canada and the United States. If it is violated, doctors can be sanctioned and even lose their medical licence, temporarily or permanently. Despite this basis for the preservation of confidentiality, the growing presence of practitioners on social media presents a risk for breaches.
Physicians, like many of us, have used platforms like Twitter and Instagram since their inception, with 90 percent reporting they used social media to find information related to their patients and practice in 2017, according to a report by market analyst Research2Guidance. Today, lists of the top twenty-five “medical influencers” include accounts of family physicians and doctors who have been endorsed by celebrities and have millions of followers. And, at times, their posts contain jokes involving patient information. A 2020 study by Wasim Ahmed of Newcastle University, which analyzed 348 tweets about living patients, found that nearly 47 percent contained details that would likely make patients identifiable to themselves.
In some ways, packaging patient information for public consumption is in line with lesser-known traditions of the medical world. The history of medicine is also a history of performance; health care workers have advanced their careers through the exhibition of less powerful people for hundreds of years. Despite the progress made around patient confidentiality during the Enlightenment, during the seventeenth and eighteenth centuries it wasn’t uncommon for both students and the public to pay an entry fee to witness dissections that took place as part of medical education in Europe. Many people viewed the practice as necessary for scientific advancement, but physicians used, almost universally, bodies of the poorest subjects, stealing cadavers from graves without consent and then displaying them for the public.
In the era before anesthetic was widely used, surgeons would operate on conscious patients before an audience of, at times, 700 to 800 onlookers. In an article for JSTOR Daily, Rebecca Rego Barry wrote that surgeons “seemed to revel in the showmanship aspect of their work,” receiving applause at the moment they entered what one medical college called the “pit.” It was this performative aspect of medicine—perpetrated by practitioners and revered by observers—that helped usher in the era of the celebrity doctor. Of course, the conditions health care professionals train and work in have always encouraged physicians to establish public influence. Canadian hospitals and medical schools reward and publicly promote their most prestigious students, researchers, and clinicians; competition for esteem and funding from donors encourages already-high-achieving people to differentiate themselves and build lucrative research reputations. But television fundamentally changed the way we think about doctors, commodifying the act of giving medical care so that it could be sold as entertainment on a mass scale.
Just look at celebrities like Dr. Drew and Dr. Oz or shows like Dr. 90210 and Botched. Every week, viewers tune in to watch the assessment, diagnosis and treatment of patients, despite the criticisms these shows have received for exploitative practices. Reality shows like ABC’s NY Med used footage from actual emergency rooms and operating theatres, sometimes filming surgeries without consent from patients. Joel M. Geiderman, an LA emergency physician, told Emergency Medicine News that he knows people who consented to being filmed while stressed and in the emergency department, then regretted the publicization of their medical treatment in the media. So, while the disclosure of medical secrets to the public is not particularly new, technology has made it much easier.
There is certainly a place for doctors online. Medical misinformation and vaccine hesitancy need to be confronted, especially in the era of COVID-19, and many clinicians have made invaluable contributions to online discussions about medical racism, homophobia, ableism, and misogyny. A number of physicians use social media to help patients with conditions underrepresented in medical literature self-advocate. Others advise oppressed patients on how to ensure they’re getting the best care possible and answer pressing questions about the pandemic.
But growing distrust in the medical establishment, which the violation of patient confidentiality encourages, must be reckoned with just as seriously. According to a recent survey by NORC at the University of Chicago, since the start of COVID, 32 percent of respondents decreased their trust in the health care system. This distrust is often particularly present in Black, Indigenous, and LGBTQ+ communities, which have been subjected to medical exploitation, experimentation, and harm for centuries. Research shows suspicion of pharmaceutical companies continues to drive vaccine hesitancy.
“COVID put physicians in the forefront of the cultural mainstream,” says Stephanie Lee, a hematologist at St. Michael’s Hospital in Toronto. “Everyone was looking to physicians for guidance on what was happening.” She adds that, for many physicians, there was a feedback loop of wanting more attention and likes on social media. While she believes health care practitioners generally have good intentions, “when the well runs dry of content on COVID, people wanted to mine their professional lives to maintain their status. COVID accelerated what was already an issue.”
The targets of these posts are, overwhelmingly, the oppressed. Faithful to the history of medical theatre, women with mental illness and patients who are geriatric, disabled, fat, impoverished, or perceived as uneducated are subjected to the majority of ridicule. And it’s not uncommon for patients in similar situations to see these posts. Reacting to discussions of trans healthcare by physicians on Twitter, one person tweeted, “My lived experience/identity has been distilled to a saccharine and self-serving Aesop[’s fable].” Another nurse, who posted that she knew when patients were faking symptoms, inspired a #PatientsAreNotFaking hashtag used by thousands of people.
“Whenever I see nurses and doctors on TikTok . . . disparaging their patients . . . it makes it hard, for not just me but a lot of people, to be vulnerable to their doctors,” says the University of North Texas’s Hermann. She adds that patients who grew up in poverty, like herself, already distrust health care professionals, and social media has the potential to make it worse. Patients have already expressed a variety of concerns in the comments sections of these platforms: “TikTok singlehandedly made me not seek medical care recently,” wrote one user; another posted about their anxieties around having emergency surgery, writing, “I was literally fearful of my nurses having their phones on them and videoing me while I’m vulnerable.” With no real oversight in place to monitor online behaviour, it’s clear that the regulations around patient confidentiality must evolve to capture these new concerns.
The Canadian Medical Association does have a data-stewardship policy that covers patient privacy, but it only mentions the sharing of patient details over email—nothing about social media. The issue has been addressed in the College of the Physicians and Surgeons of Ontario’s new set of guidelines for the use of social media by physicians, which includes the recommendation that doctors “exercise caution when posting information online that relates to an actual patient” and asks them to “bear in mind that an unnamed patient may still be identified through a range of their information such as a description of their clinical condition.” These are, however, just guidelines, and they are still violated constantly online.
Both Hermann and Lee think that social media use should be addressed in medical curricula; hospitals and medical boards already have disciplinary mechanisms in place for violations of patient confidentiality, which should be implemented when health care practitioners post derogatory content online with the same consistency that they are when practitioners are careless with physical copies of patient data. Directives, they added, should take into account that comments deriding or ridiculing sick people in general can be as harmful to the public’s relationship with the medical system as individual violations of patient confidentiality.
Lee believes that, when done correctly, patient narratives shared on social media can have a constructive and positive function. “There’s an opportunity to do a lot of good,” she says. “But physicians need to take stock of how this is really helping our patients. Is there really a net material benefit to patients by posting this? Is there an alternative way that preserves the patient’s dignity better, maintains their anonymity better?”
Asking for consent to post about a patient online is complicated, however. The power differential between patients and doctors, in most cases, is enormous. It is difficult to imagine conditions in which patients wouldn’t potentially feel coerced into agreeing to let their physician share their information on a public social media account. “Hospital fundraising campaigns share patient information all the time, but the big difference is the patients’ stories are shared after the acute issue has been resolved,” says Lee, adding that, often, those narratives are shared in the patient’s own words, sometimes written in partnership with their former health care providers. “You have to empower the patient to be part of the process, to be part of sharing their story,” she says.
In 2021, following his disciplinary hearing at the College of Physicians and Surgeons of Ontario, Martin Jugenburg was suspended from his job for six months. At some point, he removed all the patient content predating November 2019 from his Instagram account. The committee wrote that there was a “troubling pattern of Dr. Jugenburg pursuing his own interests . . . in publicity and in cultivating a strong social media presence, at the expense of the privacy of his patients.” His “seeming indifference to these issues was appalling and is deserving of significant sanction,” the committee added.
Jugenburg has since resumed his career at the Toronto Cosmetic Surgery Institute and has publicly vowed to fight attempts made by patients to seek financial compensation for the damages done. His Instagram account is still public, and he has begun posting new post-op images of his patients—presumably with permission this time. It’s almost business as usual.
For patients, the situation remains unchanged. Questions about the function of social media in medicine have yet to be posed with seriousness, and solutions have not been identified or implemented. Meanwhile, influencer-doctors continue to practise the tradition of performance, prolonging a hidden history of sickness as spectacle.
“It’s really easy to detach empathy when you’re doing a TikTok. It’s really easy for those viewers to not see that person as a person,” says Hermann. “[But] I think, now, it’s coming to a head.”







