The federal government's new COVID booster campaign is telling us it's "time to top up" by getting our next COVID booster shot.
But if you've heard the latest advice from the World Health Organization (WHO), you might be wondering if you actually need to get a booster.
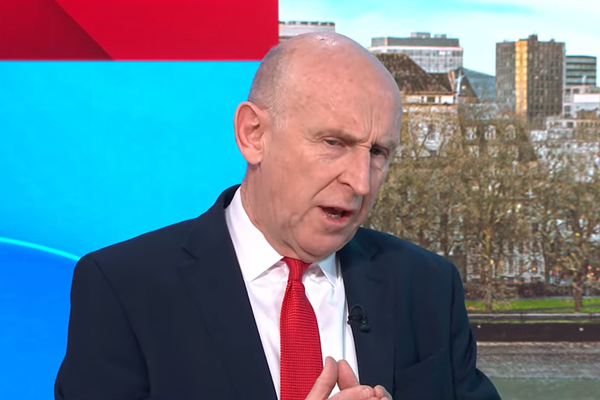
The ABC News Daily podcast caught up with University of Melbourne epidemiologist Tony Blakely to find out more.
What does the government say?
The new ad campaign from the federal government says all adults who haven't had the COVID vaccine or infection in the past six months should book in for a booster.
How is that different from the WHO?
WHO's Strategic Advisory Group of Experts on Immunization (SAGE) issued vaccination guidance in late March saying it no longer recommends COVID vaccine boosters beyond the first booster shot for adults under 50 with no underlying health conditions.
"Although additional boosters are safe for this group, SAGE does not routinely recommend them, given the comparatively low public health returns," the guidance said.
WHO still recommends all adults have the first two vaccines and one booster.
It also still recommends additional boosters for adults over 50, younger adults with significant conditions like diabetes or heart disease, people who are immunocompromised, pregnant people and frontline health workers.
Similarly, the Australian Technical Advisory Group on Immunisation (ATAGI) recommends additional boosters for anyone over 65 or younger adults with comorbidities and complex health needs.
But only asks otherwise healthy adults under 65 to consider having an additional booster.
So, if I'm under 65 with no significant health risks, should I get a booster?
Yes, says Professor Blakely — but not because it will necessarily offer you much protection as an individual.
His recent research was an economic analysis, which compared vaccinating everyone over 60 to vaccinating everyone over 30.
"It was more cost-effective to vaccinate all 30-plus-year-olds," he said.
"Why? Well, not so much because the 30- to 59-year-olds get a lot of protection themselves. But even though the vaccines are not perfect, they help reduce the transmission and therefore act as a sort of indirect protector for the elderly people and those with comorbidity."
Professor Blakely said the advice from ATAGI focuses on individual benefit rather than community protection.
"On that criteria alone, their logic stacks up," he said. "However, if you pull back and consider the whole of society, dare I use the word 'herd', then you do actually get that added benefit from vaccinating more people just to dampen the transmission. That provides that indirect or shielding type of protection for those with comorbidity.
"Now, is it right for us — as public health people and for society — to vaccinate all the younger adults to get that indirect benefit for those with comorbidity? That is a philosophical or an ethical question. You can run an argument both ways.
"But certainly in our models, you do see that this is an infectious disease. It's a contagion. So the more people that get vaccinated, even though the vaccines are not perfect at reducing transmission, they will dampen that overall transmission in the population, therefore offering indirect benefits to everyone.
"If you're over the age of 60, and if you've got comorbidities, go out there, get vaccinated. If you're less than that age, I'd still encourage it. It's not going to give you a lot of benefit. It'll give you some benefit.
"But I wouldn't be saying to people less than 60 who are fit and healthy: 'You must go out and get vaccinated'. I think that becomes more of a personal choice. But part of that personal choice, is that individual thinking about not only their own benefit, but the benefit they provide to the herd."
But is it worth risking the potential side effects of the vaccine?
Professor Blakely said although the chance of experiencing side effects like myocarditis was something to take seriously, the risk was actually quite small.
"The risk of myocarditis is not that high other than for teenage and young adult males," he said. "So that's the risk that we can identify with the mRNA vaccines, and it's really not that severe.
"[Myocarditis] is an inflammation of the heart tissue. Almost inevitably it's pretty trivial and goes away. Very seldom does it result in serious consequences, but it's definitely an increased event that happens for people — young males in particular — after an mRNA vaccine. It's very uncommon and normally very trivial."
Will getting the vaccine reduce my risk of getting long COVID?
The good news — according to Professor Blakely — is the risk of contracting long COVID is much less than it used to be.
"I can't emphasise that enough," he said. "The pre-Omicron variants were more likely to induce long COVID and when you're vaccinated, you reduce the risk further.
"There's a study out there which is getting cited everywhere which is infuriatingly saying 10 per cent of people getting COVID are getting long COVID, which is absolute bollocks."
Are we expecting to see another COVID wave over winter?
Professor Blakely thinks it's unlikely that COVID will become seasonal like the flu — at least for a while yet.
He pointed to the COVID reproduction number — also known as the R0. This number shows the number of people, on average, that an infected person will spread their illness to.
At the moment, Professor Blakely says the reproduction number for COVID is 10.
"That's a lot higher than what it is for influenza, somewhere around 2 or 2.5," he said.
"That means that it's unlikely that we're going to see this thing being seasonal for a while. It's just going to come and go based on the waning immunity in the population.
"It's going to just keep popping up whenever it feels like popping up. And my current crystal ball says anywhere between every three and five months, we'll expect to see another surge."
Listen to the full interview with Professor Blakely on the ABC News Daily podcast.