Despite intensive public health efforts to grind the Covid-19 pandemic to a halt, the recent emergence of the highly transmissible, extensively drug-resistant, and profoundly immune system-evading XBB.1.5 SARS-CoV-2 subvariant is putting the global community on edge.
What is XBB.1.5?
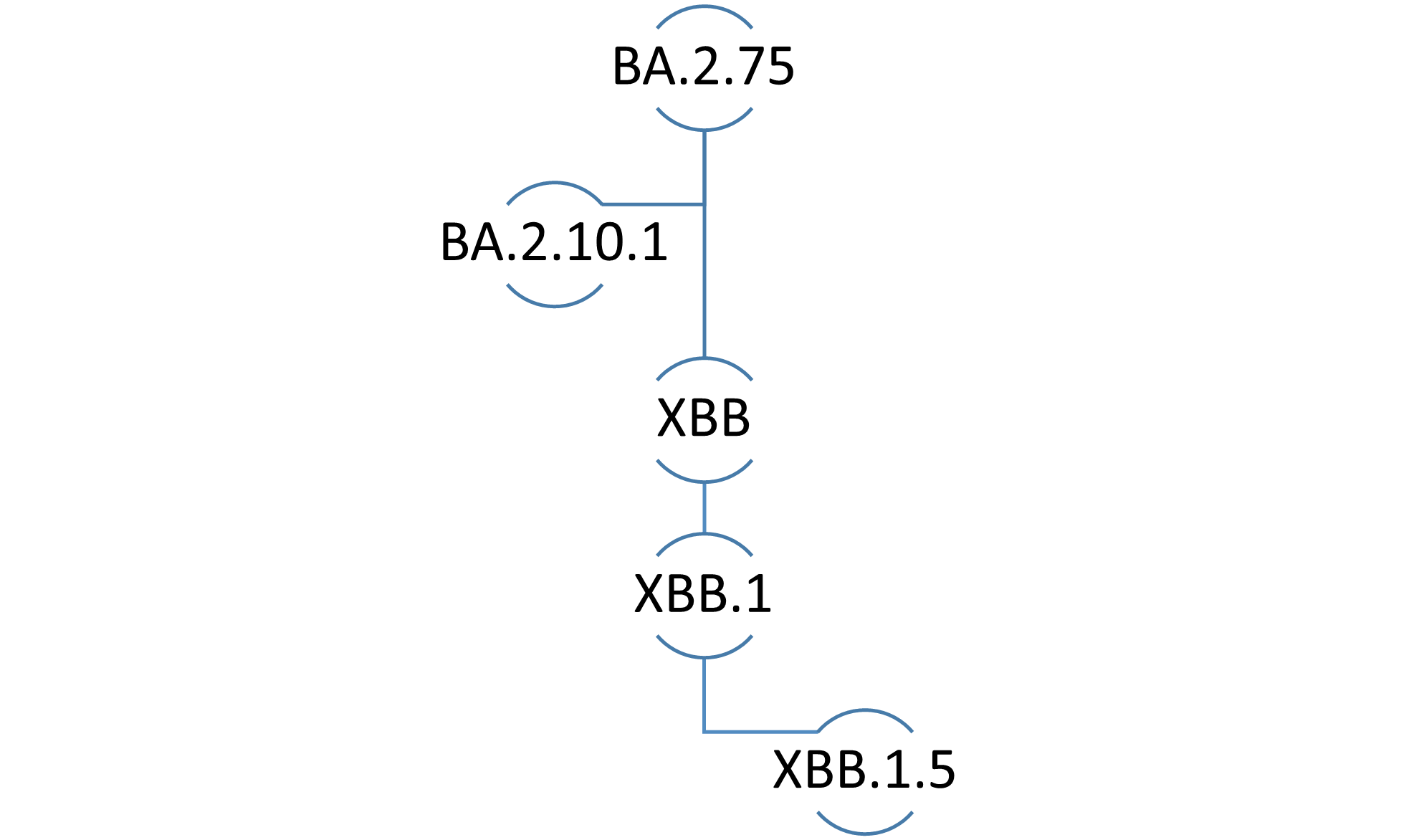
In the naming convention for SARS-CoV-2 lineages, the prefix “X” denotes a pedigree that arose through genetic recombination between two or more subvariants.
The XBB lineage emerged following the natural co-infection of a human host with two Omicron subvariants, namely BA.2.10.1 and BA.2.75. It was first identified by public health authorities in India during the summer of 2022. XBB.1.5 is a direct descendent, or more accurately, the “fifth grandchild” of the original XBB subvariant.
How does XBB.1.5 differ from Omicron?
XBB.1.5 is one of many Omicron subvariants of concern that have appeared on the global pandemic scene since the onset of the first Omicron wave in November 2021. In contrast to other descendants of the original Omicron variant (known as B.1.1.529), XBB.1.5 is a mosaic subvariant that traces its roots to two Omicron subvariant lineages.
XBB.1.5 is arguably the most genetically rich and most transmissible SARS-CoV-2 Omicron subvariant yet.
Where is XBB.1.5 prevalent?
According to the World Health Organization, XBB.1.5 is circulating in at least 38 countries, with the highest prevalence in the United States, where it accounts for approximately 43 percent of COVID-19 cases nationwide. Within the U.S., there is wide geographic variation in the proportion of cases caused by XBB.1.5, ranging from seven percent in the Midwest to over 70 percent in New England.
XBB.1.5 has also been officially reported by governmental agencies in Australia, Canada, the European Union, Japan, Kuwait, Russia, Singapore, South Africa, and the United Kingdom. Real-time surveillance data reveals that XBB.1.5 is rapidly spreading across the globe and will likely become the next dominant subvariant.
XBB.1.5 has also been detected in municipal wastewater systems in the United States, Europe, and other places.
How likely is XBB.1.5 to cause serious illness?
There is limited data about the ability of XBB.1.5 to cause serious illness. According to the World Health Organization, XBB.1.5 does not have any specific mutations that make it any more dangerous than its ancestral subvariants.
Nonetheless, XBB.1.5 is perceived as being equally capable of causing serious illness in elderly and immunocompromised persons compared to previous Omicron subvariants of concern.
Are current mRNA vaccines effective against XBB.1.5?
XBB.1.5 and XBB.1 are the Omicron subvariants with the greatest immune-evasive properties. Therefore, one of the most contentious issues surrounding XBB.1.5 relates to the degree of protection afforded by currently available mRNA vaccines, including the latest bivalent booster formulations.
Researchers from the University of Texas determined that first-generation and bivalent mRNA booster vaccines containing BA.5 result in lackluster neutralizing antibody responses against XBB.1.5. A report (yet to be peer-reviewed) from investigators at the Cleveland Clinic found that bivalent vaccines demonstrate only modest (30 percent) effectiveness in otherwise healthy non-elderly people when the variants in the vaccine match those circulating in the community.
Furthermore, some experts believe the administration of bivalent boosters for the prevention of Covid-19 illness in otherwise healthy young individuals is not medically justified nor cost-effective.
In contrast, public health experts from Atlanta, and Stanford reported that although the neutralizing antibody activity of bivalent booster vaccines against XBB.1.5 is 12 to 26 times less than antibody activity against the wild-type (original) SARS-CoV-2 virus bivalent vaccines still perform better than monovalent vaccines against XBB.1.5.
However, investigators from Columbia University in New York found that neutralizing antibody levels following bivalent boosting were up to 155–fold lower against XBB.1.5 compared to levels against the wild-type virus following monovalent boosting.
This suggests that neither monovalent nor bivalent booster vaccines can be relied upon to provide adequate protection against XBB.1.5.
How can you protect yourself against XBB.1.5?
The rapid evolution of SARS-CoV-2 continues to pose a challenge to the management of Covid-19 illness using available preventive and therapeutic agents. Of note, all currently available monoclonal antibodies targeting the spike protein of SARS-CoV-2 are deemed to be ineffective against XBB.1.5.
Antiviral medicines such as redeliver and Paxlovid may be considered for the treatment of eligible infected patients at high risk of progressing to severe disease.
Standard infection control precautions including indoor masking, social distancing, and frequent handwashing are effective measures that can be employed for personal and population protection against XBB.1.5 and other subvariants of concern.
Although bivalent boosters may be considered for elderly, immunocompromised, and other risk-averse individuals, their effectiveness in preventing Covid-19 illness due to XBB.1.5 remains uncertain.
Why is XBB.1.5 nicknamed “Kraken?”
Some scientists have coined unofficially-recognized nicknames for XBB.1.5 and other SARS-CoV-2 subvariants of concern, arguing that they are easier to remember than generic alphanumeric designations.
The “Kraken” label for XBB.1.5 is currently in vogue on social media sites and news outlets, and the nicknames “Gryphon” and “Hippogryph” have been used to denote the ancestral subvariants XBB and XBB.1, respectively. Kraken refers to a mythological Scandinavian sea monster or giant squid, Gryphon (or Griffin) refers to a legendary creature that is a hybrid of an eagle and a lion, while Hippogryph (or Hippogriff) is a fictitious animal hybrid of a Gryphon and a horse.
Notwithstanding their potential utility as memory aids, the use of nicknames or acronyms in formal scientific discussions should be avoided.
This article was originally published on The Conversation by Sameer Elsayed at Western University. Read the original article here.







