Your support helps us to tell the story
A cheap and widely accessible antidepressant has been shown to be “unexpectedly effective” in treating aggressive brain tumours, scientists have found.
The drug, named vortioxetine, costs around £40 and is usually prescribed for adults who have major depressive episodes.
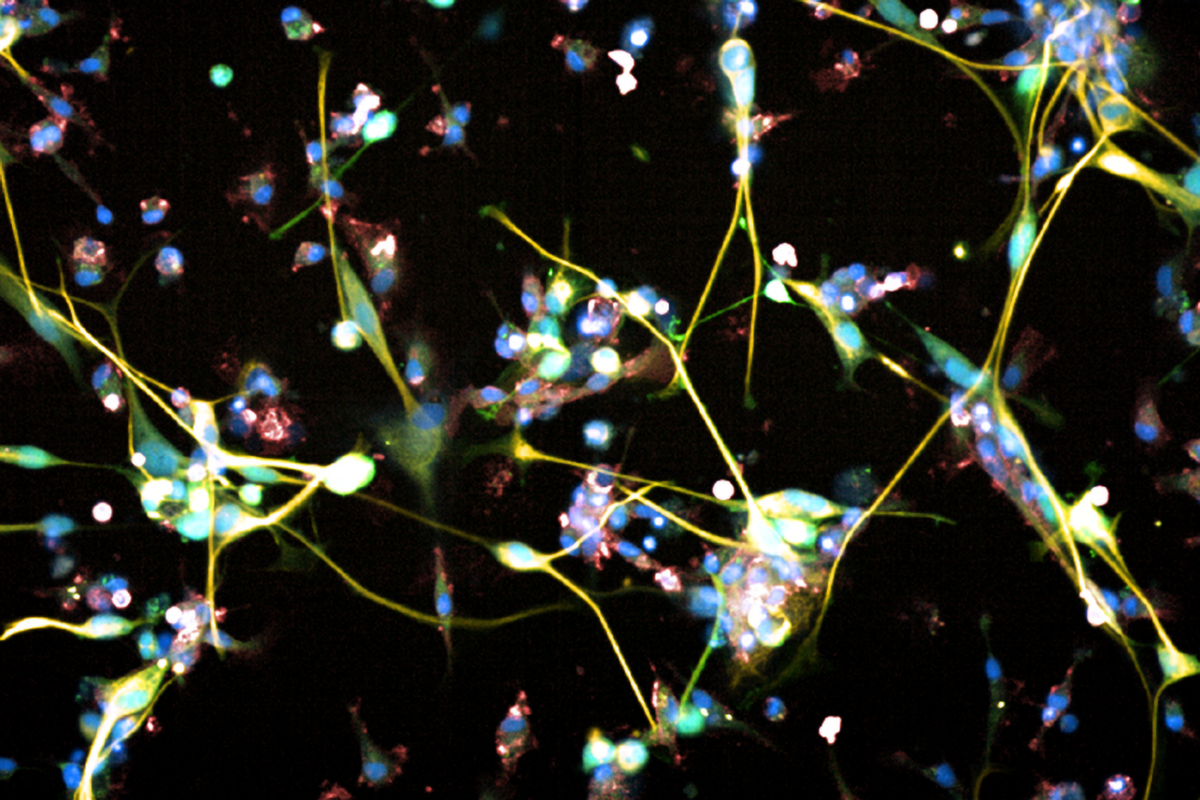
However, lab tests on cancer cells have shown it was effective in treating glioblastomas – the most common and fast-growing type of brain tumour.
Glioblastomas are the most common type of cancerous brain tumour in adults, with around 3,200 diagnosed a year in the UK.
The researchers from University Hospital Zurich have now raised hope for treating the aggressive disease, which currently has a survival time of just 12-18 months.
Further tests on mice showed vortioxetine has “good efficacy”, especially in combination with standard treatment such as surgery, chemotherapy and radiation, the scietists added.
Michael Weller, professor at the University Hospital Zurich and director of the Department of Neurology, said: “The advantage of vortioxetine is that it is safe and very cost-effective.
“As the drug has already been approved, it doesn’t have to undergo a complex approval procedure and could soon supplement the standard therapy for this deadly brain tumour.”
Only 25 per cent of glioblastoma patients survive more than one year, which goes down to 5 per cent after five years.
Drugs that are effective against brain tumours are hard to find, as many cancer drugs cannot cross a toxin-preventing membrane, known as the blood-brain barrier, to reach the brain.
As part of the study, published in the journal Nature, the researchers tested hundreds of other existing medicines that are able to cross this barrier, such as antidepressants and Parkinson’s medication.
Vortioxetine, which costs around £40 for a pack of 28 tablets, proved to be the most effective of all the antidepressants that were tested, the researchers said.
The team is looking to recruit patients as part of a clinical trial where they will be given vortioxetine alongside standard treatment.
However, academics are advising against patients trying the drug for themselves without medical supervision.
Prof Weller said: “We don’t yet know whether the drug works in humans and what dose is required to combat the tumour, which is why clinical trials are necessary.
“Self-medicating would be an incalculable risk.”
Commenting on the study, Dr Simon Newman, chief scientific officer at The Brain Tumour Charity, said: “Any scientific developments that bring us closer to new treatments for glioblastoma are promising, as treatments haven’t changed in decades.
“We urgently need kinder and more effective therapies for people facing a glioblastoma diagnosis, so using new technologies and repurposing existing drugs may help achieve this.
“Finding drugs that cross the blood-brain barrier is a particular challenge, so using drugs that we already know can do this is an exciting prospect.
“Translation of these early findings to patients most in need is the next step, and we look forward to following future studies using vortioxetine.”
Additional reporting by PA







