Where should investment be made today in order to save the maximum number of lives from cancer tomorrow? That is the underlying principle behind the “cancer groundshot” philosophy.
Annually, billions of dollars are spent on ambitious “cancer moonshot” programs. These programs focus on the discovery of new drugs and technologies aimed at solving the cancer burden. The hope is that discovery of a new target, a new drug or a new mechanism will help to cure cancer or reduce the cancer burden.
The United States’ ambitious Cancer Moonshot program marks its fifth anniversary in 2022, and certainly, cancer is still very much a global problem that needs addressing. Some new drugs have been developed in this time frame, but the percentage of patients who has benefited from these newer drugs has remained small.
Globally, most patients with cancer die not because they don’t have access to these newer drugs, but because they do not have access to even the basic treatments.

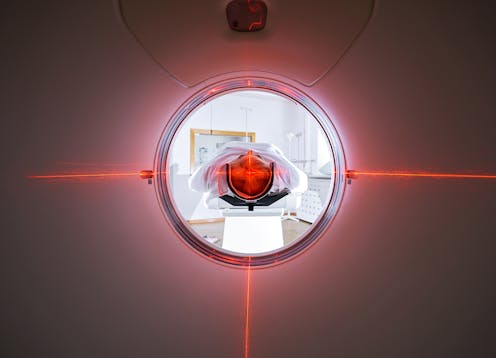
More than 90 per cent of patients in low-income countries, and more than half of patients in low- and middle-income countries, do not have access to basic radiotherapy services. More than half of patients globally who need cancer surgery will go without, and services needed for accurate cancer diagnosis are lacking.
These are interventions that help cure cancer and save the most lives, as opposed to newer drugs that only marginally extend survival or delay cancer growth. If inequity in access to proven effective interventions persists, newer treatment options will not reduce global cancer burden.
Cancer groundshot
I coined the term “cancer groundshot” in 2016 in a blog post to encourage prioritization in cancer care and research. It is a part of the common-sense revolution in oncology.
Cancer groundshot highlights that investing in improved access to interventions already proven to work saves more lives than discovery of a new intervention. When patients are dying due to lack of access to surgery or accurate diagnosis, a new cancer drug is not going to solve the problem.
Cervical cancer is a good example. It is probably the only cancer for which elimination is a realistic goal. HPV vaccination, cervical cancer screening and effective treatment of early detected cervical cancers may help us eliminate this cancer.
At the same time, newer drugs like pembrolizumab reportedly improve two-year survival rates in metastatic cervical cancer by 10 percentage points. While not discounting this medical advancement, it is more prudent for countries around the world to invest in cervical cancer screening, HPV vaccination and early treatment, rather than investing in access to pembrolizumab (one year of this drug costs roughly US$150,000).
In this example, the use of pembrolizumab represents the cancer moonshot approach to cervical cancer. Focusing on vaccination, screening and early treatment represents the cancer groundshot approach.
Costs and priorities
The cost of pembrolizumab is not an outlier. Modern cancer treatments are quite expensive. On average, based on 2018 data, a new cancer drug costs more than US$150,000 per patient per year. On the other hand, barring a few good drugs, the benefits these drugs provide are not very impressive on average. For example, some new cancer drugs delay progression by a median of only three days.

Although valuation of life is inherently an impossible task, I think as a society we can agree that our resources can be better allocated than spending $16,000 per month for delaying tumour growth by three days. A new study shows that these extra days of delayed tumour growth may not necessarily mean good quality of life, either.
Cancer groundshot is a philosophy that calls for prioritization of strategies in global cancer control. The underlying principle of cancer groundshot is that one must ensure access to interventions that are already proven to work before focusing on the development of new interventions. We need to realign our priorities and invest on equitable access to high-value interventions.
This is not only an issue in low- and middle-income countries. Severe disparities in access to care exist within high-income countries as well. There are several pockets of population in countries like the United States and Canada, that are underserved and lack access to timely and adequate cancer care. There are disparities in socio-economic status, awareness levels, insurance coverage and other factors that lead to differential outcomes, even within the same country.
Advocacy and implementation
I laid out the details of the cancer groundshot philosophy in a 2018 paper in the journal Lancet Oncology. Since then, it has been gaining momentum in the cancer policy world. I have spoken about this at several international and national meetings, and this concept has been discussed both in academia and beyond. This year at the Annual Meeting of the American Society of Clinical Oncology (ASCO), the world’s largest oncology conference, I am chairing a session on cancer groundshot.
This recognition from ASCO will certainly add to its recognition, and hopefully, adoption. The session is organized into three talks, which have also been compiled into a book chapter:
Cancer groundshot and how clinical trials fit into this philosophy.
Disparities in low- and middle-income countries, and if technology can help address this challenge.
Disparities in cancer care within high-income countries.
However, the real metric for the cancer groundshot is implementation of the philosophy and reduction in the inequities in access to proven therapies. Advocacy is the first step to achieve that end.
Bishal Gyawali receives funding from Ontario Institute for Cancer Research and Conquer Cancer Foundation.
This article was originally published on The Conversation. Read the original article.







