
Leading clinicians have called on the government to help tackle Britain’s “growing cancer emergency” after figures showed there have been around 8,000 excess deaths due to delays in diagnostics and treatment since March 2020.
Ministers are accused of failing to accept “the true scale of the problem” within cancer services in the aftermath of the Covid pandemic and are being warned that excess deaths will continue trending upwards without signifcant intervention.
In a paper published in the Lancet Oncology journal, experts called on officials in the Department of Health and Social Care to apply the same levels of focus and urgency deployed during the vaccine roll out to cancer services, in what they describe as a “watershed” moment for the country.
They said that NHS data for November showed that, “in the last 12 months 69,000 patients in the UK have waited longer than the recommended 62-day wait from suspected cancer referral to start of treatment”.
This was twice as many than in 2017-18, they said.
While the whole cancer pathway “seems overwhelmed”, there are some areas such as radiotherapy that are now “critical threatened”, the cancer experts warned.
They quote European research data suggesting there has been a 17 per cent increase in UK cancer deaths due to delays in diagnosis and treatment.
They also cite statistics showing “excess cancer deaths since March 2020 are already 8,815 with 3,327 in the last six months, and this trend is likely to continue”.
The paper also sets out the solutions presented by frontline clinicians that can prevent excess deaths if the government and NHS take action, as well as some of they problems they face.
The paper says that, “currently some front-line staff are exhausted and too afraid to speak out, never mind feel part of the solution” and warns that “inefficient practices have emerged”.
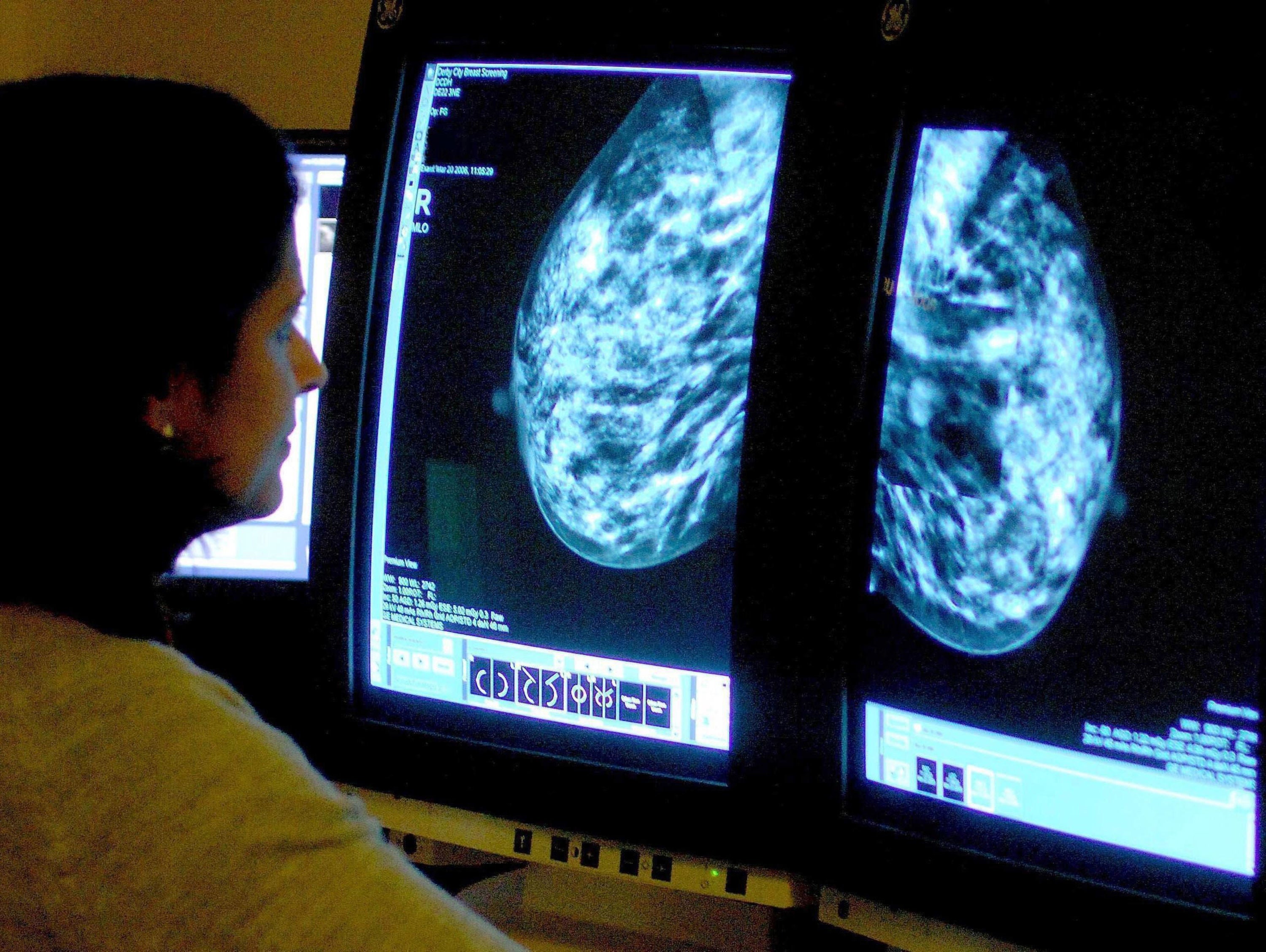
It states: “Secretarial support [has been] suspended so consultants are less productive than they should be, obsolete IT is slowing every day work, workflow tools not being purchased and antiquated equipment such as radiotherapy machines so out of date they take twice as long as modern machines to treat patients less well than is possible.”
Professor Pat Price, founder of the #CatchUpWithCancer campaign and a leading oncologist, said: “This is a watershed moment for UK cancer services - the biggest cancer crisis ever - we can’t accept the normalization of record-breaking cancer treatment waiting times.
“Clinicians know it doesn’t need to be this way and that we don’t need new groundbreaking research to avert disaster.”
He added: “We need a radical new plan, investment in capacity solutions in treatments like radiotherapy, and the political will to treat more patients on time. If ever there was a time for us to deliver much needed investment into cancer treatment it is now.”
Professor Gordon Wishart, former cancer surgeon and chief medical officer of Check4Cancer said: “The Covid-induced cancer backlog is one of the deadliest backlogs and has served to widen the cracks in our cancer services.
“Readers will be shocked to learn that even before the pandemic, the UK was near the bottom of the cancer survival league tables.”
He added: “Now we face a deadly cancer timebomb of treatment delays that get worse every month because we don’t have a sufficiently ambitious plan from policymakers. I urge the government to work with us.”
Dr Amar Ahmad, a general practitioner based in Wilmslow, said: “It’s very clear that Britain is in the midst of a growing cancer emergency. Just as there was a concerted national effort to tackle the Covid Pandemic, we need a similar national drive to address the declining state of cancer diagnosis and treatment in the UK.”
He added: “Freeing up frontline clinicians from needless box-ticking NHS bureaucracy will go some way to improve the NHS capacity to tackle this emergency.”
At the end of last month, Steve Brine, the Conservative MP and chair of the health and social care committee, said he would make tackling cancer backlogs a priority and questioned whether the government still intended to bring forward a new cancer treatment plan.
In February, the then-health and social care secretary, Sajid Javid, called for evidence to underpin a new 10-year cancer plan for England.
But Mr Brine questioned the future of the plan, a document he first published as a health minister in 2019.
The DHSC previously said it was “working at pace to improve outcomes for cancer patients across England, including by improving referral rates – during August, 92 per cent of people started cancer treatment within a month of referral.”
The spokesperson added: “We have also opened over 90 community diagnostics centres so far, which have delivered over two million additional scans, tests and checks.
“We received 5,000 responses to our call for evidence to inform a new cancer plan, and next steps will be set out in due course.”







