Depression is one of the most common mental health conditions, yet different people can experience it in contrasting ways. For example, depression influences how one eats in divergent ways: Some people lose their appetite entirely, while others feel insatiably hungry.
Scientists estimate that among people diagnosed with major depressive disorder, about 48 percent will experience decreases in appetite, while roughly 35 percent experience increases. Yet there’s little scientific evidence to help explain why some people feel one way and others the opposite.
New research on the brain’s reward system could help move the conversation forward — and may even help improve depression treatments. The research fits with a number of studies that tie food and mental health together.
Depression, appetite, and the brain
Earlier research suggests that depression-related appetite changes may stem from neural and inflammatory differences between people diagnosed with different kinds of depression. This study, published in August in the journal JAMA Psychiatry, focused on the brain and examined the relationship between appetite changes and the reward system.
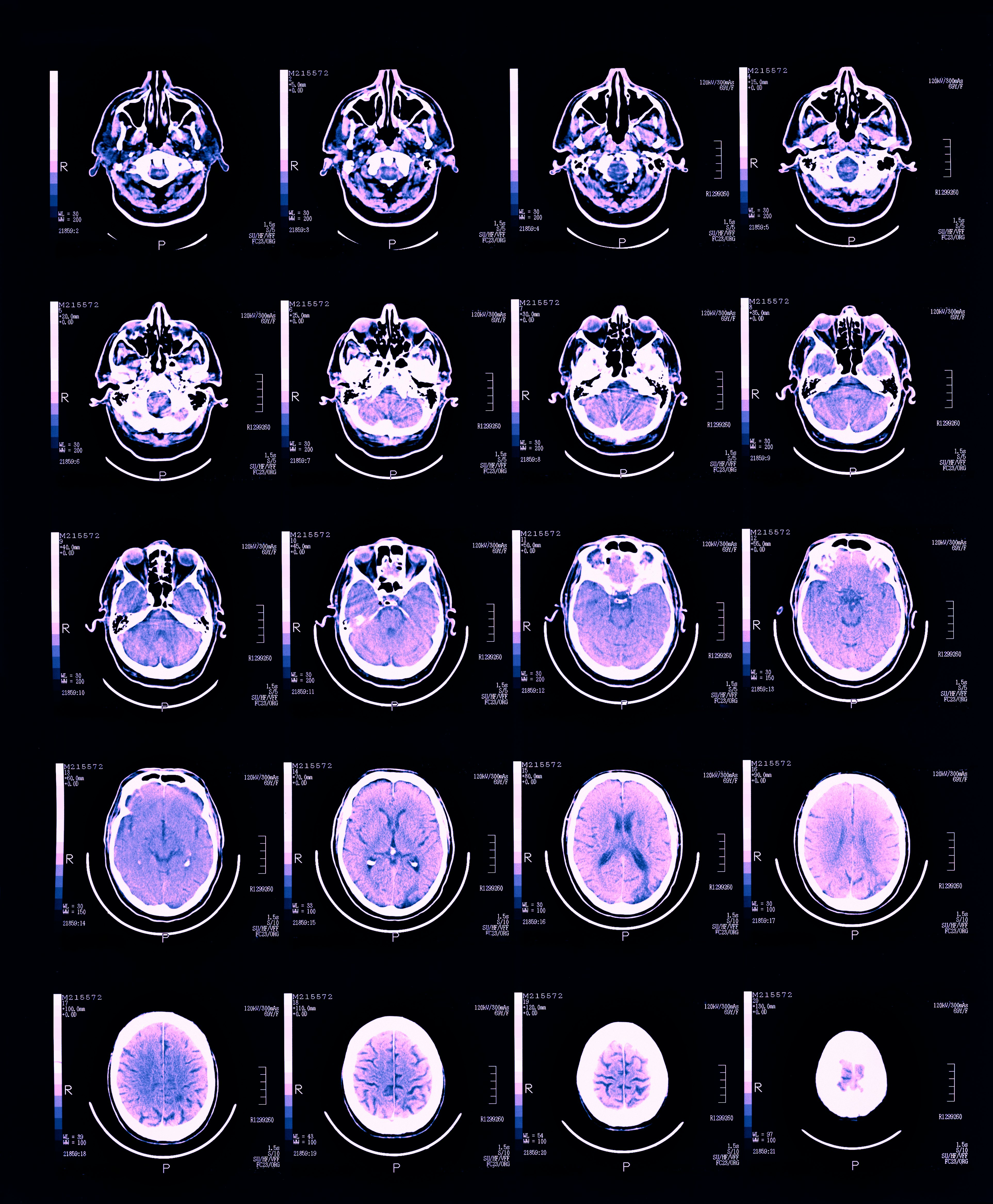
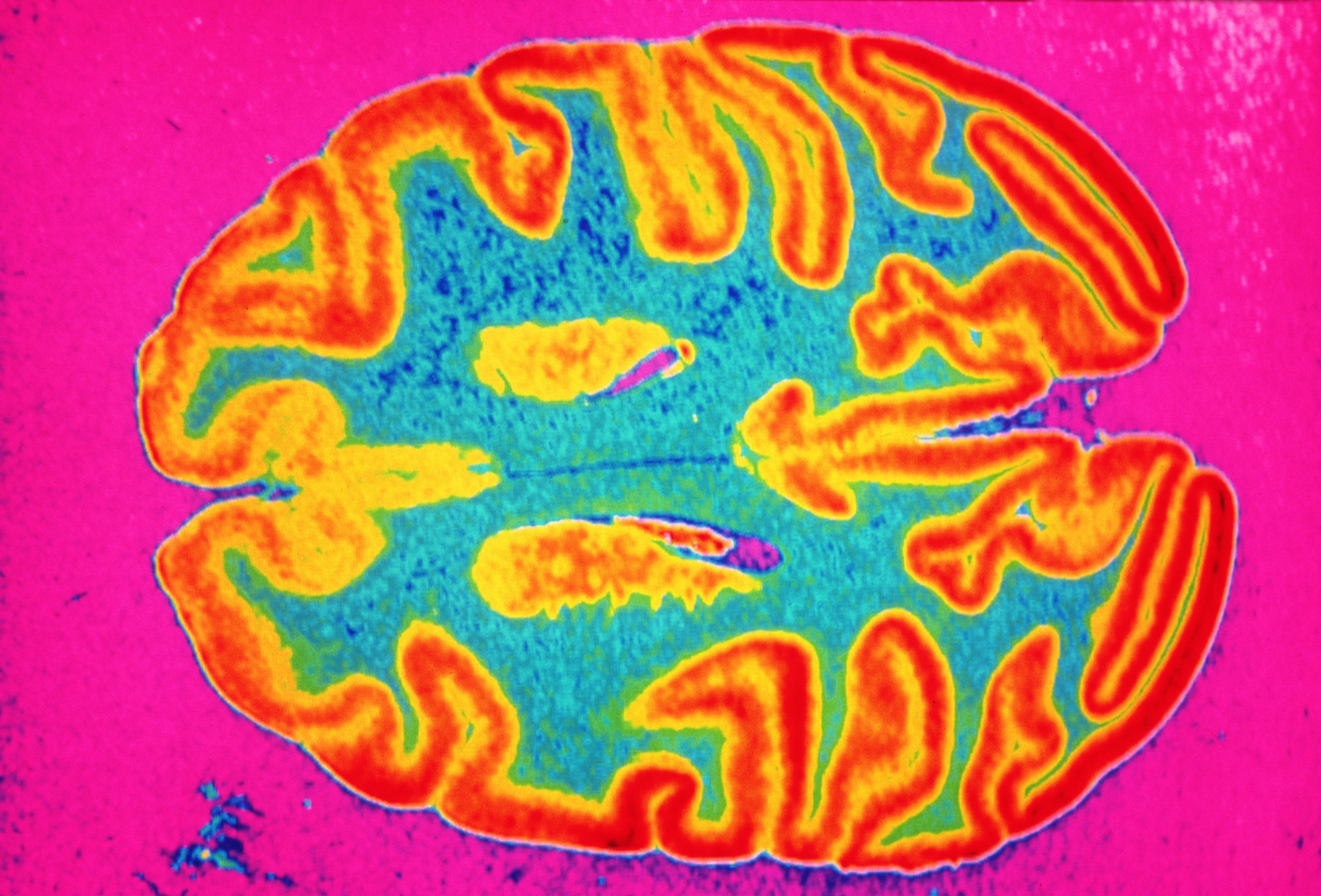
Ultimately, scientists found that the direction of appetite changes — an increase or a decrease — matched specific neural alterations. For example, reduced appetite in individuals with depression was associated with weaker communication between the brain’s nucleus accumbens, ventromedial prefrontal cortex, and hippocampus. Meanwhile, increased appetite was linked to weaker communication between the nucleus accumbens and the insular ingestive cortex. The nucleus accumbens is directly involved in motivation and emotion.
What’s more, the scientists found that the more severe an individual’s symptoms, the more robust the neural signature. The changes were so prominent among individuals with severe depression that the team could predict whether or not the study participant experienced an increase or loss of appetite based on their brain.
But it’s still unclear why depression causes these changes, explains first author Nils Kroemer, an associate professor of medical psychology affiliated with the University of Bonn and the University of Tübingen. Further, while it’s possible that depression results in these differences, there’s also the possibility that these deviations result in depression.
Future treatments for depression
The different ways that people experience depression also makes it hard to understand the exact neurobiological mechanisms that lead to it, explains Kroemer. That said, he hopes this study “will inspire more work on narrower dimensional symptoms instead of the categorical diagnosis of depression.”
“I think we need to characterize changes in reward function much more thoroughly at an individual level so that we can better identify effective treatments based on emerging insights of neurobiological mechanisms,” Kroemer says.
An individual-based approach is referred to as precision psychiatry. It’s possible that improved identification of reward system changes could allow scientists to use targeted brain stimulation to alleviate symptoms of depression. Next, Kroemer and his team plan to pursue elements of this idea and test how non-invasive vagus nerve stimulation can target the gut-brain axis and improve mental health.
In the more immediate, people looking for ways to combat depression could find relief from an appetite-related source: food. A poor diet is also associated with depression, while a healthy one is linked to a reduced risk of developing it.
In 2019, scientists examining young adults with depression found that the study participants put on a three-week diet intervention experienced fewer depression symptoms at the end of the trial. This diet was similar to the Mediterranean diet; participants were encouraged to increase their intake of vegetables, fruits, wholegrain cereals, nuts, olive oil, and protein.
Research also suggests healthy diets can improve the success rate of other depression treatments, like medication and therapy. If you are feeling depressed, please reach out to your medical provider, as well as your trusted support system.