Anthropogenic climate change is turning ambient heat, a relatively banal manifestation of the sun, into an inevitable environmental hazard. In 2023, with the atmospheric carbon dioxide level reaching new heights of 425 ppm, we witnessed the warmest decade on record spanning from 2014 to 2023. Until a few decades ago, hazards of high heat largely existed in confined, fire-based occupational settings or for people who exerted in hot weather for a long time, e.g. soldiers, athletes, and workers, and during occasional heatwaves.
Mentions of heat stroke have been found in literature since ancient times. With rising global temperatures, dangerous high heat has begun permeating our routine indoor spaces. This gradual expansion of the realm of extreme heat is potentially the gravest consequence of climate change for India.
India has observed a significant mean temperature increase of 0.15 degrees C per decade since 1950, according to a 2020 assessment by the Ministry of Earth Sciences. The observed warming is not occurring evenly across India. Warm days and warm nights have also increased at about seven and three days per decade, respectively, during the period 1951-2015. Currently, 23 States, mainly of plain and coastal regions, are considered more vulnerable to widespread heat impact. However, that doesn’t mean hilly states are safe. Although their maximum temperatures do not reach heatwave threshold levels of 45 degrees C, the population is experiencing higher temperatures compared to previous decades.
Heat stress and heat stroke
Exposure to severe or continuous heat leads to heat stress. When uncompensated, heat stress manifests as heat-related illnesses. Such illnesses range from superficial/mild and manageable (e.g. prickly heat, heat-related swelling, heat cramps, heat exhaustion) to a medical emergency (i.e. heat stroke). Heat stroke is the most severe of heat-related illnesses: it presents with impaired brain function (i.e. stroke) due to uncontrolled body heating. It is a time-critical condition that often turns fatal if there is a delay or failure in reducing body temperature by rapid, active cooling. Besides neurological impairment, high core body temperature (at least 40 degrees C), or hot, dry skin are other heat stroke symptoms. These may be confused with fever. Clinically, a diagnosis of heat stroke poses a unique challenge as it requires the elimination of other causes of stroke, history of infection, and medication overdose.
There are two types of heat stroke. Exertional heat stroke is seen in young, fit individuals performing strenuous physical activities in hot or outdoor environments. It develops within one to two hours of exertion, especially when physical efforts are unmatched by physical fitness, even at moderately high temperatures. On the other hand, relatively slow-developing classic heat stroke is often difficult to fathom, challenging to identify instantly, and deadlier. Observed in individuals lacking the ability to regulate body temperature, e.g. children, the elderly, the sick, and the disabled, this heat stroke is more common during heatwaves. It contributes to about 9-37% of heat-related fatalities during heatwaves, and hence is also called epidemic heat stroke. Importantly, it occurs in hot environments in the absence of strenuous physical activity as individuals fail to perspire or cool off.
Heat stroke is different from other medical conditions in that it does not require the transmission of a virus or bacteria from one person to another, nor does it need the violence of physical trauma that may occur from a gunshot, fall, or due to a cyclone. Someone in perfect health and participating in what seem to be normal activities may die from heat stroke within an hour.
Pathophysiology of heat
The heat-related illnesses mentioned above are not the only cause of emergency or mortality during hot summer days. Normal human body temperature stays within a narrow range of 36.3-37.3 degrees C. It maintains thermal balance through radiation (40%), evaporation (30%), convection (27%), and conduction (3%). Any external or internal condition that increases body temperature invokes various physiological responses changing cardiovascular, kidney, and metabolic systems, driven by increased blood flow to the skin and dehydration.
A review of the pathophysiology of heat-related illnesses found 27 different pathways that lead to mortality through various combinations of vital organ damage and pathophysiological mechanisms. As such, cardiovascular followed by respiratory, renal, and other chronic causes rank as the most common causes leading to increased emergencies and mortalities during hot days. Hence, estimating the increase in emergency attendance and all-cause deaths during summer has become an easy, practical tool to assess the impact of heat on the population. Cases and deaths that occur solely due to heat stroke represent just the tip of an iceberg.
Heatwaves’ compound effects
Heatwaves are among the deadliest natural hazards. Apart from the aforementioned direct impacts, there are also multiple indirect health impacts due to disruption in services (power, water, transport), increase in food and water-borne diseases, increase in drowning and accidents, and due to overburdened/slowed health services. Globally, thousands of people die yearly and many suffer livelihood consequences due to heat. However, the full impact of a heatwave is often difficult to realise fully until weeks or months later.
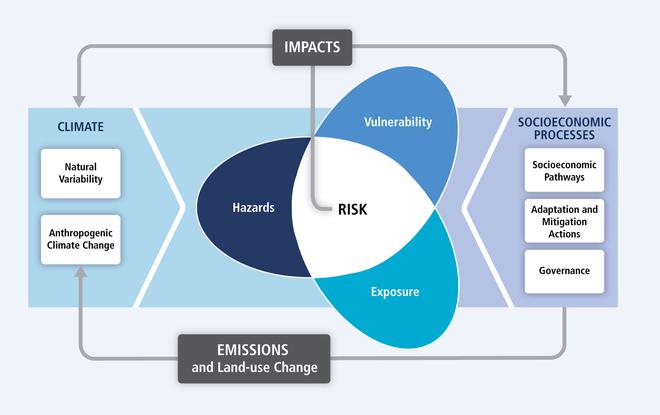
That is not all. Heatwaves also have compound and cascading environmental impacts like concurrent drought, glacial lake outbursts causing flash floods, urban/wildfires, and increased air pollution from ground-level ozone and dust storms. Due to the potential to create widespread health and economic damage, heatwaves can be categorised as a disaster. The disaster risk triad framework delineated in the U.N. Intergovernmental Panel on Climate Change’s Fifth Assessment Reports (2014) can explain its health impacts in that context.
Understanding heat exposure
Multiple physical, socio-economical, environmental, and institutional factors determine health outcomes of heat exposure at the population level. In assessing it, using the disaster risk triad – hazard, exposure, and vulnerability– concept, the first and foremost challenge comes in estimating the exposure.
Conventionally, maximum daily temperatures have served the purpose. For example, thresholds for announcing heatwave and severe heatwave warnings for plain areas of India are at maximum temperatures of 45 degrees C and 47 degrees C, respectively. Although the role of high humidity in amplifying heat stress has been recognised, most available heat indices are not adequate for estimating our population’s risk. One widely used heat index (maximum temperature and humidity) equation was formed decades ago, before climate models existed, with assumptions and perceptions of different levels of temperatures among healthy, western individuals. It is also found to be underestimating the severity of heatwaves. The wet bulb globe, which mirrors how the human body cools itself with sweat in outdoor conditions, has been a promising measure. The quest for finding and validating a suitable index for the Indian population is very much on.
Epidemiologically, it is important to note: first, in the current scenario, whichever threshold is used to announce heatwaves, the health impacts of heat on the population do not begin to occur only after those threshold temperature levels are crossed. Health impacts begin much before, even at moderate temperature levels. In terms of external factors, humidity plays a crucial role in creating heat stress by limiting our body’s major cooling mechanism: sweating.
Even at moderate temperatures, like 35 degrees C, if the relative humidity is 70%, it will feel like 50 degrees C to us. In terms of internal factors, heat’s impacts depend on the acclimatisation and build-up of heat stress in the human body. Acclimatisation is a gradual physiological adaptation (short-term) that increases heat tolerance as a person incrementally exerts in a hot setting for a few days. Air conditioning and comorbidities reduce our heat tolerance. Similarly, long-term adaptation occurs in people living in hotter regions over the years. Therefore, tourists from colder regions are particularly at risk of heat stroke when they visit hotter regions.
For example, people living in Ahmedabad might be more adapted to high temperatures than those in Varanasi. In a study of city-level daily mortality, all-cause deaths in Ahmedabad seem to increase after maximum and minimum temperatures crossed 42 degrees C and 28 degrees C, whereas in Varanasi, they increased after 33 degrees C and 27 degrees C. Both physiological adaptations take time to develop. Hence, exposure to sudden extreme temperatures is dangerous for anyone, even healthy and young. The heat-related deaths in Maharashtra in April 2023 highlighted the dangers of heat.
Second, not everyone has the same heat exposure at a particular recorded temperature. For example, frail, elderly, living alone, living on the top floor, and not having active cooling were some risk factors associated with heat-related deaths reported during the 1995 Chicago heatwave. Cities retain more heat because of the geometry of built-up building material, concentrated human activities, and lack of vegetation, leading to higher night-time temperatures than the surrounding rural areas. This urban heat island effect contributes to continued heat exposure among city dwellers who, especially, lack sufficient means of active cooling, e.g. fans, air conditioning, and cold drinking water. High night-time temperature has emerged as a significant predictor of heat-related mortality.
A study conducted in Kolkata in the summer of 2019 found that indoor heat index levels in urban slum dwellings were 5.29 degrees C higher than that outdoors. Dangerously high heat and humidity (at least 45 degrees C) remained for an average of about nine hours/day in urban slum dwellings compared to 2 hours a day in rural houses. These differences were particularly notable at night. During the coolest time of night, the insides of urban dwellings recorded a 6.4 degrees C higher heat index than outdoors, while the insides of rural houses recorded 1.3 degrees C above outdoor levels. Cement walls, clay tiles, corrugated tin roofs, fewer rooms, and crowding made urban slums dangerously hot.
Similarly, a study from Ahmedabad recorded an average 6.7 degrees C higher heat index at the locations where patients with acute heat illnesses were picked up by emergency medical services compared to what was recorded by the nearest weather station during the summer of 2016. At the city level, such differences translate into an increase in all-cause mortality with daily city temperature. Hence, city-level temperature-mortality study has become vital for heat-health action planning.
Children and pregnant women are particularly vulnerable. Higher heat production, greater body surface area, lower sweat production, underdeveloped physiology, lack of risk perception, and poor water replenishment make children, especially infants, more vulnerable to heat impacts. Each 1 degree C temperature increase is associated with reduced birth weight and a 5% increase in the risk of preterm birth and stillbirths.
Although air conditioning helps, relying on it for our cooling needs only multiplies our existing problems of urban heat islands and global warming. Therefore, the focus should be given to passive cooling inside buildings through better ventilation, window shading, reflective paints, suitable building materials, and traditional methods. At the urban level, understanding heat hotspots, increase in green-blue structures, access to cool spaces, support for suitable adaptation measures, and multisectoral health-centric heat action plans are relevant.
Heating up the puzzle
Because of the multifaceted dimensions of heat impacts, assembling pieces of the population heat exposure puzzle is complicated especially as warming continues. However, understanding existing vulnerabilities and taking action to prevent extreme heat’s impact is very much in our hands. And importantly, heat-related illnesses are preventable. Assessing patterns of socio-economic, demographic, and environmental factors, access to basic services, disease distribution, existing institutional mechanisms, and preparedness helps to take stock of the situation and to prioritise resource allocation for vulnerable populations, and strengthen institutional responses.
Governance, health workforce, vulnerability and adaptation assessment, integrated risk monitoring and early warning, climate-resilient and sustainable technologies and infrastructure, management of environmental determinants of health, and climate-informed health programmes are some of the components for building climate-resilient health systems, according to the World Health Organisation.
Public health action
Adaptation measures to extreme heat are essential and urgent as our actions in this decade have the potential to change the course of irreversible planetary consequences. The window for action is closing fast. Because emitted greenhouse gases (GHG) will continue global warming until carbon levels are settled, even after net zero may be achieved, a health-centric adaptation focus should be seriously followed in every sector. This will also help us stay on course for the Sustainable Development Goals.
In the health sector, the National Programme on Climate Change and Human Health (NPCCHH), a health programme of the Ministry of Health and Family Welfare, technically supported by the National Centre for Disease Control, works to achieve goals envisioned in the ‘Mission on Health’ under the Prime Minister’s Climate Council. Since its launch in 2019, the programme is carrying out its mandate to increase general awareness, build the capacity of health professionals and strengthen the health sector to respond to changing disease patterns and to withstand increasing extreme weather events in the context of climate change.
Many of these measures reach communities and health facilities across the country through an organisational structure under NPCCHH that includes nodal officers in states and districts in health departments and the army of medical officers and community health workers. It is trying to address multiple climate-sensitive health issues with a priority focus on the health impacts of heat, other extreme weather events, air pollution; vector-borne and water-related illnesses in the context of climate change; and green and climate-resilient health facility infrastructure.
Extensive awareness efforts, cascading training of health professionals, early warning dissemination, and integrated health surveillance are the key activities being carried out under the programme. The programme launched the National Action Plan on Heat-Related Illnesses in July 2021. Advisories for the general public (including “do’s and don’ts”) and for state health departments for health sector preparedness are issued through the health ministry at the beginning of the summer every year. National heat-related illness surveillance focuses on heat stroke, emergency admissions, and cardiovascular and all-cause mortalities as reported by health facilities.
Globally, the health sector contributes to about 5.2% of the carbon footprint, and India’s health sector is the seventh largest contributor. So apart from various adaptation measures, efforts are also directed towards reducing GHG emissions from the health sector, under the NPCCHH, through measures like energy efficiency, renewable energy transition, passive cooling like cool/green roofs, water conservation, and rainwater harvesting, among others. After all, mitigation is the panacea for climate change.
India is highly vulnerable to climate change impacts. It is the third largest emitter of GHG currently. At the current global warming of 1.2 degrees C, frequent, intense, and expansive heatwaves are no longer a prediction. They are becoming a painful reality. According to a recent assessment, the April 2023 heatwave in India was made 30-times more likely by climate change. With the El Nino settling in, the coming years might witness record-breaking summers. It will only worsen if we collectively fail to control GHG and knowingly slide towards the inevitable 1.5 degrees C mark. Without an immediate reduction in fossil-fuel-based energy which powers our buildings, vehicles, agriculture, supply chains, and many basic services, we will be ensuring future global warming and its wider impacts on our health and life of future generations. Let’s pledge to reduce our impacts on the environment.
Our every action counts!
Dr. Purvi Patel is a public health specialist with experience working in the area of climate change, heat and health.







