
By 2048, 40 percent of those aged 65 won't own their own home, a vital tool in accessing care
Widely understood for millennials and younger, the Retirement Commissioner’s three-yearly retirement income policy review details a housing crisis for those 65 and above.
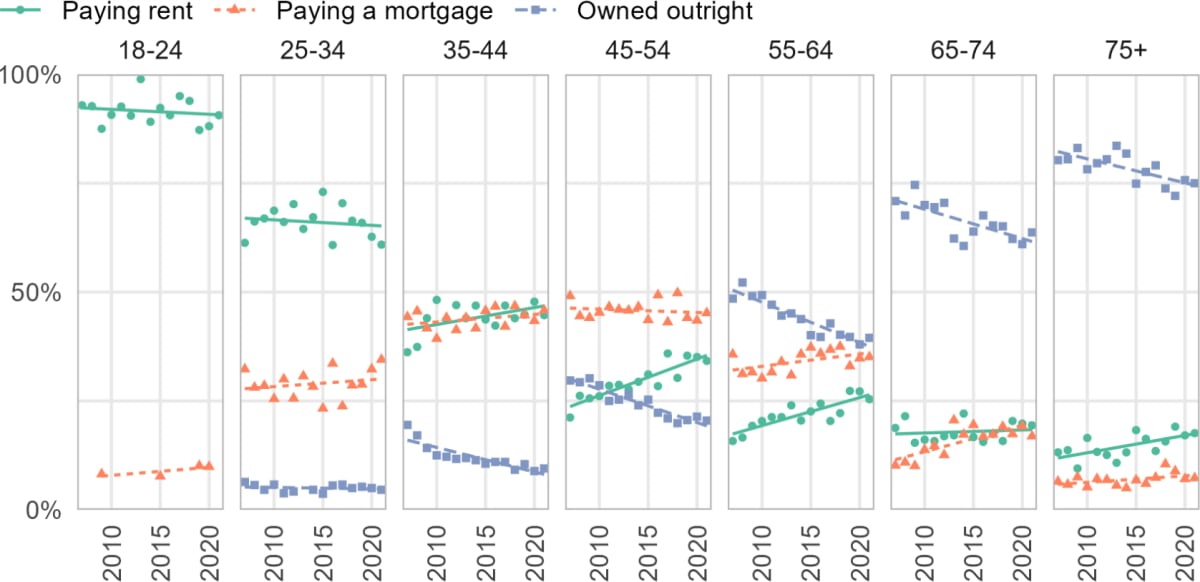
Jane Wrightson’s report says if current trends continue there will be a 100 percent increase in people renting aged 65 in the next two or three decades.
“This is a staggering projection that will change New Zealand’s housing landscape. Long-term the balance of homeownership is expected to shift to 60 percent homeowners and 40 percent paying rent. By 2048, this 40 percent will equate to up to 600,000 people.”
READ MORE: * In aged care crisis, the grass is always greener on the other side of The Ditch * A modest proposal for radical reform of community care * Retirement villages to close doors in ‘perfect storm’ of nursing shortages
Wrightson points out this doesn't bode well for New Zealand’s pension scheme which is based on the assumption retirees own their own homes outright.
Aged care facilities, which are by far the largest healthcare providers in New Zealand, are already pushed to breaking point by funding shortfalls and related worker shortages. The ageing population means the country needs another 15,000 new care beds by the end of the decade and around 40,000 in the next 20 years.
It is currently losing beds due to nursing shortages, and the vast majority of those that are being built either attract a premium above government funding in exchange for superior accommodation or are built as part of a continuum of care for major retirement players such as Ryman, meaning securing a care bed means first purchasing a retirement unit.
The retirement village model is built around home ownership, and funding for care above government funding requires having some equity or cash in the bank. Being New Zealand, this means having a home to sell.
Parallel issues
Aged Care Commissioner Carolyn Cooper said, “I am concerned that housing and health are parallel issues and many times when people's housing, or the environment they live in, is not suitable their health suffers.”
Cooper said there were 650 care homes in New Zealand and quite a few still catered for people relying on government subsidies to access care.
Aged Care Association chief executive Simon Wallace said the Retirement Commissioner’s report was a “wakeup call” for what an ageing population meant, and any work required for 20 years’ time had to begin now, likely with a review of the funding model to move it away from relying solely on premiumisation or on retirement villages to build the care units as a loss leader to sell village units.
However the aged care industry did have a major win last week in the form of pay parity for its nurses, meaning providers can effectively compete with the much higher paying Te Whatu Ora/Health NZ for staff.
Wallace said the move, which begins in the middle of next year, was a great step forward but wasn’t enough to reopen the 1260 care beds that had closed due to staff shortages this calendar year, many of them in already under-serviced rural communities.
Cooper acknowledges the lack of affordable/solely government-funded care units going forward but said the forecasts assumed things were going to continue to be done the way they were now.
Community care
“We need to think of different ways of actually looking after older people as they age, including looking after them in a more comprehensive way in their own homes and actually not relying on aged residential care as heavily unless it is necessary.
“That should allow for equity, particularly for populations that don't traditionally access aged residential care in the same way, Māori and Pasifika particularly, who may also be living in less favourable conditions at home.”
Around 75,000 older and disabled people access home and community support currently and the number is expected to grow in line with population, though Cooper said it was also experiencing workforce shortages.
“We're going to have 20 percent of the population over 65 in just over 10 years time. So planning for health and disability services and appropriate housing is all really important and I'm not seeing as much planning in that area is we need to have.”
“It's just a fact for the future and we need to plan for it. We need the right health system, we need the right housing system, we need the right financial system to actually ensure that older people, as they age, actually have the quality of life and quality of care that they deserve.”






