
The genetic risk of developing Alzheimer’s disease is more strongly influenced by the mother’s side than the father’s side, a recent study has discovered.
Alzheimer’s disease steals memories, independence and the capacity to connect with loved ones. In 2020, over 55 million people worldwide were living with dementia. Alzheimer’s disease is the most common form of dementia, accounting for 60-70% of all dementias.
It’s expected the number of people affected by dementia will nearly double every 20 years. Finding ways to better diagnose, treat and even prevent dementia is more important than ever. This latest study could provide a useful target for researchers hoping to develop new therapies.
The study, published in JAMA Neurology, showed that people whose mother had a history of memory loss had a greater risk of developing Alzheimer’s disease at any age when compared to people with only a paternal history of memory loss (or no family history of memory loss whatsoever). However, if a person’s father had early-onset memory loss (occurring before the age of 65), they also had a greater risk of Alzheimer’s disease.
The study analysed data from 4,413 people aged 65 to 85 who had no issues with cognitive function or memory problems. The study’s large sample size is a key strength, making for a more accurate interpretation of the findings compared to previous research. But it’s important to note it’s not a complete representation of the population, as most participants were white – so results may differ in other ethnicities.
The participants were part of the Anti-Amyloid Treatment in Asymptomatic Alzheimer study, which is a phase 3 clinical trial investigating a drug researchers hope will slow the progression of memory problems. The participants’ cognitive function was measured using questions from the widely used mini-mental state examination.
Positron emission tomography (PET) imaging was also used to scan their brains for markers of Alzheimer’s disease and determine their risk of developing it.
The researchers were mainly looking for the presence of amyloid plaques, which are one of two hallmarks of Alzheimer’s disease. These toxic amyloid plaques form when protein pieces, called beta-amyloid, clump together.
The hypothesis is that these clumped amyloid plaques are the prime suspects in damaging and killing brain cells (neurons), resulting in Alzheimer’s disease. The second hallmark of Alzheimer’s is the protein tau, which wasn’t assessed in this study.
The accumulation of beta-amyloid is thought to be a prominent precursor of Alzheimer’s disease, as people can have raised amyloid levels years before memory problems start.
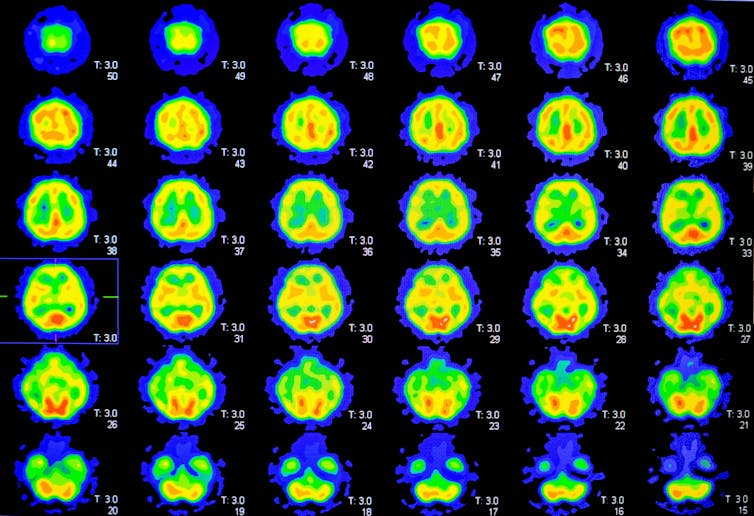
The results of the PET scans showed that participants whose mother had a history of memory impairment (regardless of the age her memory problems started) had higher beta-amyloid levels. The amyloid levels were significantly higher on average in those with maternal history than paternal history of memory impairment.
Participants whose fathers had early-onset memory loss (occurring before 65) also had higher beta-amyloid levels. In comparison, participants who only had a paternal history of late-onset memory impairment (happening after 65 years of age), and those who had no family history of memory loss, had normal beta-amyloid levels.
The reason for this link is not completely understood.
One suggestion from the researchers is mitochondria dysfunction. Mitochondria are energy-providing structures inside our cells. These are only inherited from the mother’s side. Mitochondria possess their own DNA, which may include mutations that cause them to malfunction. Previous research has already demonstrated mitochondria dysfunction is associated with Alzheimer’s disease.
Read more: Alzheimer’s disease: problems with the brain’s energy supply could be a cause
The brain is an energy-hungry organ, taking up about 20% of the body’s energy. So it’s unsurprising that dysfunction in mitochondria could lead to cognitive impairment – and potentially Alzheimer’s disease.
Developing treatments
This study builds on previous, smaller studies which have investigated the role genetics play in Alzheimer’s disease. Since these studies only had small sample sizes, they lacked the statistical power to draw strong conclusions. This study’s much larger sample size allowed for stronger conclusions and reaffirmations on the importance of maternal genetics to be made.
The key message from the study is that a person’s risk for Alzheimer’s disease could depend on whether they inherit it from their mother or father, as well as their parent’s age when memory loss began. As such, considering gender-specific parental history could be fundamental in identifying those at greatest risk of Alzheimer’s.
In light of these findings, next steps could be to determine whether the DNA from the mother – specifically the X chromosome itself – influences the disease’s development. If it does play a role, then researchers may have a better target for treatment.
And given mitochondria are inherited from the mother’s side, researchers may also want to further investigate the mitochondria dysfunction theory to better understand if this explains why people are at greater risk of developing Alzheimer’s disease if their mother had memory problems.
Read more: Can Alzheimer's really be reversed, as a new documentary claims?
This latest study confirms the critical role that genetics play in the development of Alzheimer’s disease. But it isn’t the only risk factor. Many modifiable risk factors – such as diabetes, high blood pressure, cardiovascular disease and poor diet – are also known to be massive contributors to developing the disease.
Rahul Sidhu does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article was originally published on The Conversation. Read the original article.






