LOS ANGELES — Los Angeles County is already in the grips of a coronavirus surge fueled by the omicron subvariant BA.5, but yet another worrisome strain that’s causing concern in India has also been found locally.
Designated BA.2.75, the subvariant is being monitored by the World Health Organization. As of Thursday, six cases had been identified in the U.S., including two in California, with one of those in L.A. County, according to county Public Health Director Barbara Ferrer.
“It does appear to have additional mutations that facilitate spread and evade immunity,” she said during a briefing. “And it’s been spreading fairly rapidly across India.”
Scientists are exploring whether the emergence of BA.2.75 could eventually prolong or exacerbate the existing surge now being fueled by BA.5 — another highly infectious member of the omicron family.
“Whenever there’s an identified new variant of concern, or in this case a lineage that’s under monitoring, we do need to proceed with caution, as it takes time to better understand the risks that may be posed by this newly mutated virus,” Ferrer said.
Over the weeklong period that ended Saturday, BA.5 made up an estimated 65% of new cases nationwide, according to the U.S. Centers for Disease Control and Prevention.
“I hope BA.5 sticks around, because then people will have some reprieve and then the curves go down,” said Dr. Peter Chin-Hong, a UC San Francisco infectious diseases expert. “But if BA.2.75 (spreads), that adds another variable in the mix,” he added, raising the possibility that “you’ll see a whole bunch of people passing different things back and forth, and they’ll get something that they didn’t get before.”
A dizzying number of subvariants have emerged since omicron first landed on California’s shores around Thanksgiving. Just since April, three different subvariants — BA.2, BA.2.12.1 and now BA.5 — have been estimated to be the dominant strain nationwide.
That, in turn, has made it possible for people to get reinfected within a relatively short time frame. Since the start of the pandemic, some people have reported getting infected two, three, even four times.
“It takes time to determine with certainty the ability of a newly mutated virus to evade immunity protections to easily infect others and to cause severe illness,” Ferrer said. “Until we have a sense of how the virus is interacting with us with these new variants, using sensible precautions remains a very good idea.”
Previously, scientists had suspected that people who were infected with the coronavirus had several months of particularly strong immunity to protect against reinfection. But now, some people are reporting getting reinfected within a span of several weeks.
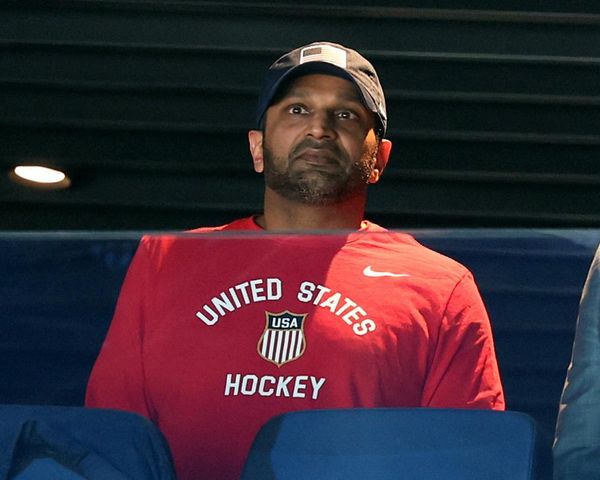
One of them is Xavier Becerra. The secretary of the U.S. Department of Health and Human Services tested positive in Sacramento in mid-June — about 3½ weeks after initially testing positive while visiting Berlin.
Getting reinfected with the coronavirus may increase long-term health consequences over time.
Even just one infection with the coronavirus is associated with increased risk of long-term death and other symptoms of illness.
A reinfection was associated with additional risk of death, hospitalization and adverse health outcomes, affecting things such as the cardiovascular, gastrointestinal, neurological and kidney systems; and increasing risk of diabetes, fatigue and mental health disorders, according to a preprint study written by scientists with the Washington University School of Medicine and the Veterans Affairs Saint Louis Health Care System.
The additional risk of reinfection was shown both in unvaccinated and vaccinated people, and was present not only in the acute phase of illness, but persisted in the months after the initial infection resolved.
Most risks “were still evident at six months after reinfection,” the report said, which surveyed the medical records of veterans, including nearly 39,000 people who had two or more infections, 257,000 who had one infection, and more than 5 million people without a record of infection.
“Assessment of the cumulative risks of repeated infection showed that the risk and burden increased in a graded fashion according to the number of infections,” the report said. “The constellation of findings show that reinfection adds non-trivial risks of all-cause mortality, hospitalization, and adverse health outcomes in the acute and post-acute phase of the reinfection.”