The Government will be hoping a suite of new initiatives can produce the 1600 extra health workers a year New Zealand will need to keep pace with population growth projections
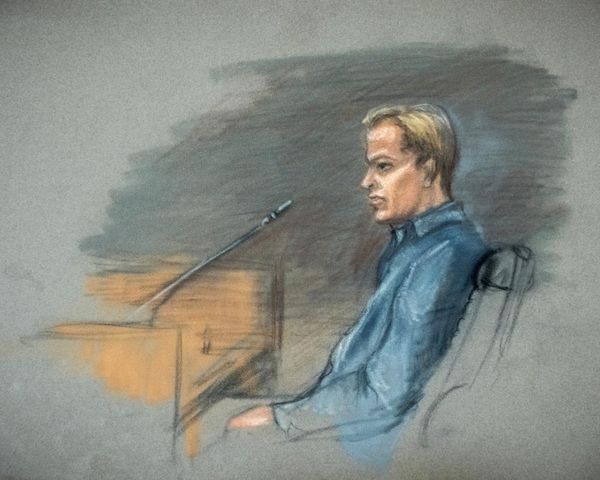
Minister of Health Ayesha Verrall has unveiled plans to recruit or train 1600 more health professionals a year and turn around training and retention issues in the health sector.
That's the number of health workers Te Whatu Ora predicts the country will need to keep up with projected population growth.
READ MORE:
* Verrall flexes health system's muscles
* Aged care 'deliberately' underfunded
But while getting there will require some big shifts, tertiary health educators say they are delighted that universities are being involved in the decision-making process.
Professor Warwick Bagg of the University of Auckland’s faculty of medical and health sciences said the plan was a first for the sector.
“We think this is excellent because for the first time we have got a long-term target of where the gaps are and how we are going to get there,” he said.
“We haven’t had a long-term health workforce target like this previously, and it gives us the clear ability to aim our efforts to work together.”
In Verrall’s words, this plan is a diagnosis a year on from the introduction of health agencies Te Whatu Ora and Te Aka Whai Ora.
Shifting demographics also mean the plan will need to focus more on Māori and Pasifika recruits, with both groups' representation in the health workforce needing to nearly double in the next decade in order to reflect what the population is expected to look like.
And while filling the gap of some 8000 workers is the most pressing need, a swelling population would only see the need for robust recruitment and healthy retention grow.
Bagg said tertiary educators had been asking for a plan like this for a long time.
“It’s fantastic to have the ministry diagnose the problem, now we know the target we need to aim for.”
Bagg said a focus on roles like pharmacy prescribers could also help take the load off the system. These are pharmacists able to write prescriptions, increasing community access by allowing some people to bypass a visit to the doctor’s office.
It’s a role that gained prominence worldwide during the pandemic as pharmacists were given starring roles in vaccination rollouts.
Bagg said it's been a “welcome expansion” that relieves pressure on the system.
However, pharmacy prescribers require a postgraduate qualification that many have to achieve while working.
Bagg hoped the Government’s plan to expand training pathways for 50 additional pharmacy prescribers per year would improve accessibility for pharmacists once delivered next year.
These form part of 135 new training places each year for other health jobs, in theory providing the country with a fresh supply of paramedics, oral health therapists and radiation therapists.
Other initiatives in the plan are an increase to ‘earn-as-you-learn’ programmes, expanding access to cultural and hardship support for Māori and Pacific students in training and establishing funding for Māori providers to take more students on placement and to offer increased training and development roles.
Associate Minister of Health Peeni Henare said it was important Māori could see themselves in the health workforce given their current significant under-representation prevented them from accessing culturally-safe and responsive care.
“We know Māori students have higher rates of attrition in training than non-Māori, non-Pacific students – and one of the reasons for this is financial hardship, meaning they have to leave programmes late in training,” Henare said.

“Training in health can be a full-time affair, particularly in later years; it asks a lot of students and their whānau. It’s a huge waste of talent and investment for New Zealand if these students leave – so this plan will expand access to hardship support to help those students stay in training through to completion.”
But the Opposition says it’s a diagnosis of a problem the current Government allowed to take seed.
National’s health spokesperson Dr Shane Reti called it a “half-baked announcement” that focused on bureaucracy rather than the front line.
“Labour has been in Government for the last six years and has failed to address the health workforce crisis that has unfolded in that time, under their watch,” he said.
“And with the workforce now in crisis, Labour is desperate to make it look like they’re doing something but it’s all too little, too late.”
National’s plan if elected is to pay nurses and midwives student loan repayments if they enter a bonding agreement of five years, and make New Zealand a more attractive destination for workers from overseas.
Bagg said retention was a complex issue, and that health workers shouldn’t necessarily be discouraged from spending time abroad.
“Many New Zealanders want to spend some time overseas, and we encourage that because they bring back new skills,” he said. “The problem is the long-term loss when they don’t come back, and that relates to salary differentials for example with Australia, and we’re never going to win that battle.”
He said the answer was to make sure New Zealand’s health sector was a safe and rewarding place for people to work.
Te Whatu Ora has already implemented a voluntary bonding scheme, which had 488 applicants this year.
The scheme offers financial incentives to health workers in exchange for being sent to areas of the sector with the most need. These included 204 nurses now working in mental health and addiction, and 71 midwives in the country’s hardest-to-staff communities.